By Stephanie Breitbart and Liz Madison, Vitals contributors
Eighteen years ago, Kim Watson took her first steps inside a hospital as a registered nurse. There were many unknowns in that moment. Perhaps one consideration that didn’t cross Watson’s mind was how she and millions of other healthcare workers would face a pandemic head-on in less than two decades’ time.
The challenges and stresses of the pandemic are everywhere and happening all at once—again and again. In healthcare, it is no different, and now it comes courtesy of the Omicron variant. But there are those like Watson who continue to answer the bell for another round in the fight. And miraculously, they have seen opportunity in the face of the opposition.

Kim Watson, nursing director of Sutter Medical Center, Sacramento’s ICU.
Watson is no stranger to the rapid pace of an intensive care unit, caring for some of the most critically ill around the clock. She started her nursing career in 2004 in a pediatric ICU. Over time, her responsibilities grew. She is now the nursing director of Sutter Medical Center, Sacramento’s 24-bed intensive care unit—a position she took on in 2018 before anyone had heard of a virus called COVID-19.
Watson responded early when faced with constantly changing circumstances that COVID-19 brought to her unit along with an increased number of critically ill patients. But rather than feel discouraged, she viewed what some may see as constraints and got creative. Working within local, state and federal guidelines, she developed clear and efficient tools for her staff so they could better support care of patients.
“The pandemic forced me to change my focus from some of my daily administrative responsibilities and think of what do my staff need at this moment to provide the best care for our patients,” she said. “I couldn’t address everything, but I listened to my staff and could make changes to ensure they had the right equipment, education and tools required to continue to give excellent care to our patients.”
Personal protective equipment remains top of mind for ICU and other clinical staff. As supplies fluctuated early in the pandemic, Watson implemented a tool inside the ICU called a “Stoplight Report.” It allowed staff and clinicians to see the status of critical PPE supplies at a glance. The real-time data kept staff up to date, but also provided them reassurance on efforts underway to secure needed items.
Watson’s critical-thinking skills in response to COVID also helped create efforts with long-lasting implications beyond the pandemic. Watson redesigned carts that are stocked with the necessary supplies and equipment to address “code blues,” where patients experience unexpected cardiac or respiratory arrest and require immediate help to resume breathing. The redesign included ways to minimize aerosol exposure—important for helping reduce spread of the COVID-19 virus. These carts remain in use for adult and pediatric patients and are still taken to every code blue at Sutter Medical Center, Sacramento today.
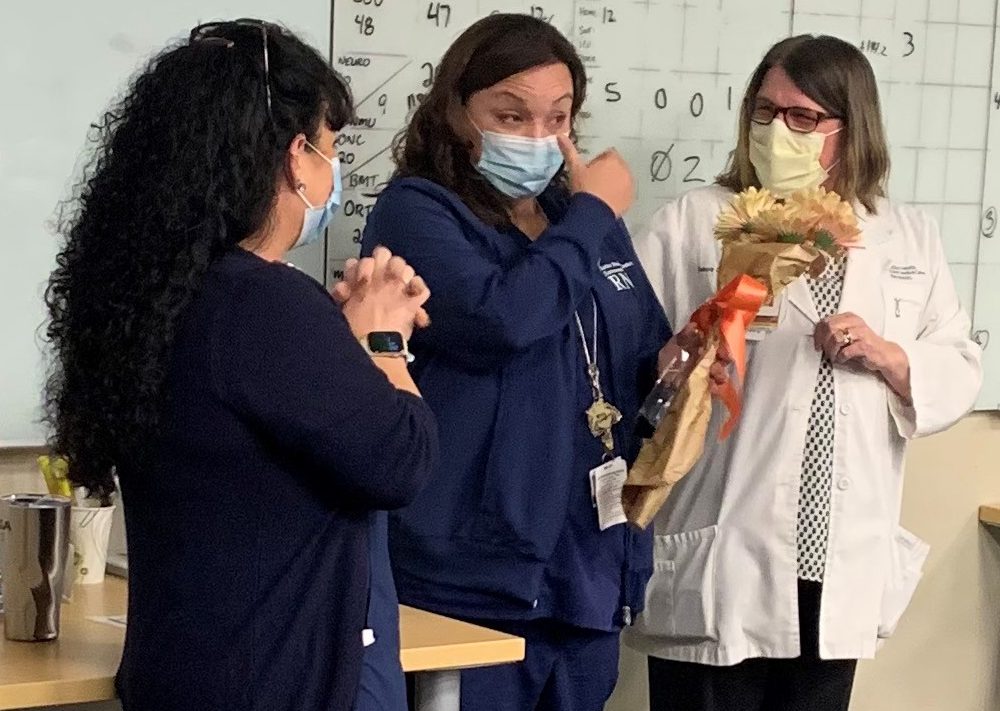
Kim Watson is congratulated by colleagues Stephanie Johnson, left and Debi Cale, right, for her nursing award recognition.
“In the middle of the pandemic, Kim was so creative,” said Stephanie Johnson, who oversees critical care and emergency services at Sutter Medical Center, Sacramento. “She pulled things out of her hat that we didn’t know could be done. I am so proud of Kim and can’t thank her enough for how well she supports our patients and our teams.”
Watson recently earned recognition for her approach to nursing, along with three other nurses from across Sutter’s network, out of nearly 300 individual nominations. But to her, it’s not about the kudos. It’s about the collaboration that helps her team continue to respond with resiliency.
“These were not just my ideas. It was about listening to my staff and together coming up with operational solutions that are real and can be applied,” she said. “It’s about going to the people who do the work, asking them what they need and figuring out how we can implement it.”





