When John Crews held his newborn grandson for the first time, he couldn’t stop smiling. For years, Parkinson’s disease had made that moment impossible, until deep brain stimulation (DBS) surgery at Sutter Health gave him back control.
“I remember looking at my daughter, who had tears in her eyes. It was the first time I’d been able to hold one of my grandbabies,” said Crews, now 62.
Crews’ Parkinson’s symptoms began when he was just 40 – two decades earlier than most people are diagnosed. The Granite Bay, Calif. resident, a former BMX racer and longtime bike shop owner, spent years relying on his cycling community for support as tremors worsened.
“I couldn’t eat in public without flinging food everywhere,” he said. “I told myself I wasn’t ready for DBS. I didn’t think my Parkinson’s was ‘bad enough.’ But eventually, my quality of life was suffering, and I knew it was time.”
Parkinson’s disease is a progressive neurological condition classified as a movement disorder. These disorders affect the brain circuits that control motion, balance and coordination. At Sutter, patients with Parkinson’s and other movement disorders are evaluated by a multidisciplinary team that includes specially trained neurologists and neurosurgeons who focus on diagnosing and managing these complex conditions.
From Breaking Point to Breakthrough Treatment
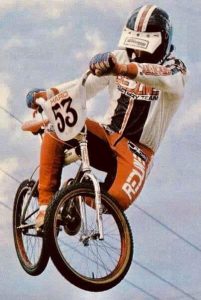
Crews, a former professional BMX racer, underwent DBS in August to help relieve Parkinson’s symptoms.
In August, Crews underwent DBS surgery at Sutter Medical Center, Sacramento, led by neurosurgeon Dr. Rudolph Schrot with support from neurologist Dr. Steven Nakano and Linda Ramatowski, an advanced practice clinician who guided him through pre- and post-operative programming.
Crews was the first Sutter patient to receive a new rechargeable DBS system, called Percept™, that detects brain activity linked to Parkinson’s symptoms and automatically adjusts stimulation in real time.
“While Sutter has long performed DBS, John’s procedure marked the first use of this system, proven in clinical trials to maintain or improve benefits for patients while reducing side effects and battery use,” Dr. Schrot said. “It’s a major advancement that helps us personalize treatment more than ever before.”
The procedure requires detailed planning and close coordination across the care team. Using advanced 3D imaging and navigation technology, the surgeons mapped Crews’ brain to identify the areas that control movement, then placed electrodes (tiny wires) that deliver gentle electrical pulses to help reduce tremors and stiffness.
“John was an excellent candidate for DBS,” Dr. Schrot said. “Our goal was to reduce symptoms enough to restore independence in daily life, and he’s achieved that.”
“DBS isn’t a one-size-fits-all solution,” added Dr. Nakano. “We partner closely with patients to determine eligibility and coordinate care across neurology, neurosurgery and rehabilitation to ensure the best outcomes – it’s truly a team effort.”
During the seven-hour procedure, Crews remained awake so the team could monitor his speech and movement. “It sounds scary, but I didn’t feel a thing,” he said. “I’ll never forget repeating, ‘It’s a sunny day in Sacramento!’ while they worked.”
“Having surgery is just part of the process,” said Ramatowski. “Success depends on teamwork, persistence and the patient’s spirit – John’s determination has been vital.”
“She coached me through it,” Crews said of Ramatowski, who stayed by his side during the procedure. “When I felt like giving up, she said, ‘You’ve got this, John.’”
Regaining More Than Mobility

Crews is a committed Parkinson’s fundraiser and advocate within his community.
Since surgery, Crews has found physical relief and renewed purpose. “My psychological outlook is better. I feel like there’s more ahead of me,” he said. “I’m thinking about getting a motorcycle again and doing an adventure ride to Utah.”
He’s back to participating in cycling events that raise money for Parkinson’s research and continues to advocate for others living with the disease.
“I probably should have done DBS a year earlier,” Crews said. “But I wasn’t ready. Now I look back and say, ‘Piece of cake.’ Would I do it again? Absolutely!”
“DBS is one of the most effective tools we have for managing complex movement disorders,” Dr. Schrot said. “At Sutter, we’re using the latest technologies, from adaptive systems to 3D imaging, helping patients like John reclaim control and return to the activities that matter most.”
Sutter’s Advanced Neuroscience Service Line offers comprehensive care for movement disorders, including DBS evaluation, surgery and ongoing support. The team coordinates with physical, occupational and speech therapy providers to ensure holistic care.
For more information, visit: https://www.sutterhealth.org/services/neuroscience.





