Rebeca Calderon of Los Banos, a rural community in the heart of California’s Central Valley, came to the small hospital in her town barely able to breathe and thinking she was going to die. She tested positive for COVID-19.
For most rural residents who are critically ill with the coronavirus, the only option is for them to be transferred to the nearest large city, where the hospitals have the right specialists and nurses to care for them. It’s a transfer that comes with risks.

The eICU has computer stations with six to eight screens that contain all the information and even real-time video shots for patients who are critically ill.
But Calderon was able to stay in her hometown hospital, with her care coordinated by intensivists and specialty nurses 200 miles away – in Sutter Health’s electronic intensive care unit, which they call the eICU, 200 miles to the north in Sacramento.
Calderon was the first patient to be cared for using an enhanced telehealth solution created specifically for a potential COVID-19 surge that now has allowed Sutter Health to help treat hundreds of patients in 20 of its hospitals throughout Northern California.
Sutter, a national pioneer in electronic ICU, has for 16 years ensured critically ill patients in both large cities and small towns have 24/7 access to an expert team of doctors and nurses specially trained in their care. From central hubs in San Francisco and Sacramento, these doctors and nurses monitor patients in ICUs many miles away using live interactive video and remote diagnostic tools. They can instantly assess critical changes in a patient’s condition and provide expert critical-care support and supervision for the hospitalists and nurses who provide the hands-on care.
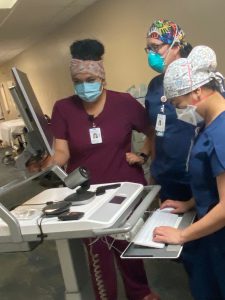
Memorial Hospital Los Banos nurses set up the eICU cart that is being used in converted COVID-19 ICU patient rooms.
“We would love to be in the hospital providing the hands-on care, but there simply are not enough critical-care providers at these smaller hospitals,” said Vanessa Walker, D.O., a pulmonologist at Sutter Roseville Medical Center and medical director of the Sutter Valley Area eICU. “It’s really difficult to transfer a patient to a larger hospital if they get really sick. With the eICU, we can keep them in their community where they have their support system and provide that same level of care as if they were in Sacramento or San Francisco.”
Said Ash Gokli, M.D., a Sutter vice president and Chief Clinical Operations Integration Officer: “The remote eICU provides critical care 24/7. By doing this we can keep patients locally and avoid transports, which improves patient safety.”
Preparing for a COVID-19 Surge
Sutter Health has more than 300 ICU patient rooms at 20 hospitals, each one outfitted with interactive video cameras. The health network’s eICU, which was first installed in 2004, was in need of an upgrade, and the new system was launched in January 2020, just before the pandemic hit.
Then, in March, in preparations for a COVID-19 patient surge, it became apparent that the eICU would need to be expanded to help care for patients in converted private rooms. Within a month, the team provided a solution. Sutter designed and deployed specialized units that enable the eICU’s intensivists and critical-care nurses to care for upward of 1,000 coronavirus patients without having to travel from hospital to hospital and using in-demand personal protective equipment.

Dr. Vanessa Walker uses six screens to help monitor and treat patients in critical-care rooms in 10 hospitals.
Sutter’s eICU team created and deployed 82 specialized iPad stands that connect to the eICU system to bring these specialized critical care teams to patients in converted COVID-19 care rooms, too.
“The challenge was to come up with a plan for our eICU to provide care for a surge in patients across Northern California,” said Dr. Tom Shaughnessy, medical director of Sutter Bay Area eICU. “We are now able to meet the need of a patient surge at our rural hospitals and large medical centers by giving the same comprehensive, quality care whether a patient is in one of our ICU beds or a converted room.”
How the eICU Helped Treat Calderon
Memorial Hospital Los Banos, with 30 licensed beds, has a single, open-room ICU with four beds and no intensivists. Often the facility’s critically ill patients require transfer to larger hospitals. Calderon was the hospital’s first severely ill COVID-19 patient, and she was placed in a private medical-surgical room that had the proper ventilation.
There, the nurses and hospitalists cared for Calderon with supervision and assistance from the intensivists and specially trained nurses in the eICU, with the aid of the new iPad system.

Rebeca Calderon of Los Banos celebrates her hospital discharge after recovering from a critical COVID-19 scare.
In helping her care for Calderon, Los Banos ICU nurse Sheila Gonzales praised the iPad system and the eICU team. “It feels like they’re right there,” she said.
Calderon recovered from the novel coronavirus and has since traveled to see friends in Texas and family in Mexico. Now hospitals throughout the Sutter network have used the system for patients who need to be isolated and still have 24/7 critical-care physician and nursing coverage.
“We have nurses and physicians providing some of the best bedside care in the country, and the eICU allows us to come in and provide advanced specialized support as they care for patients,” said Dr. Walker. “This is critical in the care for those suffering from compromised lung function due to a virus such as COVID-19. Now with these additional mobile units, we are well prepared to meet a surge of patients from this current crisis or any other that may come in the future.”