From the driving range to hospital discharge, one patient’s journey through Sutter’s coordinated stroke network.
Chris Honeck thought it would be a typical afternoon at the driving range. The 54-year-old from Rohnert Park, Calif., was still new to golf and eager to get in a few swings, but just minutes in, something felt off.
“It was like my arm wasn’t connected to my body,” he recalls.
At first, Honeck brushed it off as dehydration. But when his words became jumbled and his speech began to slur, his instructor asked if they should call 911. Honeck agreed.

Chris Honeck, 54, prepares for a swing shortly before he began exhibiting signs of a stroke. (Rohnert Park, June 2025)
That quick decision triggered a seamless, behind-the-scenes chain of events at Sutter Health, one designed to deliver expert stroke care with speed and precision.
From the moment paramedics arrived on scene, trained Sonoma County Emergency Medical Services, EMS, professionals began evaluating Honeck for stroke symptoms. They alerted the Emergency Department at Sutter Santa Rosa Regional Hospital while still in the field, giving hospital first responders precious minutes to organize and prepare. By the time Honeck arrived, Sutter’s stroke response team was ready and waiting. Emergency physician Dr. Nicholas Peairs began the initial evaluation while Honeck was wheeled from the ambulance into the hospital hallway.
Honeck was next moved to a CT scanner, where neurologist Dr. Noureldin Abdelhamid connected through Sutter’s virtual telestroke network and reviewed his brain scans in real time.
The diagnosis was a large clot in the left middle cerebral artery, a vessel critical for speech and motor function.
Thanks to Sutter’s stroke protocols, developed through years of teamwork and training, Honeck was swiftly given a powerful clot-busting medication called Tenecteplase, or TNK. And because of the severity of his stroke, the telestroke team also simultaneously began arranging his transfer to Sutter’s CPMC Davies Campus in San Francisco, where he could receive more advanced care. They alerted the hospital’s neurointerventional radiology team and a CPMC neurologist right away, so they’d be ready in case he needed a specialized procedure called a thrombectomy to remove the clot.

Nobl Barazangi, MD, PhD
“There was no pause in Chris’ care because every part of our stroke system moves in parallel,” said Dr. Nobl Barazangi, a neurologist, stroke specialist and chief of stroke care at Sutter Health. “From EMS to the ER to the telestroke consult, the transfer center and the rapid response teams at both hospitals – everyone had a role, and everyone delivered.”
By the time Honeck arrived at CPMC, the clot had begun to dissolve. Surgeons stood ready, but the procedure was ultimately not needed. Hours later, Honeck regained his speech; although, he was still experiencing some sensitivity in his right hand, affecting his finger dexterity.
With his condition improving, Honeck was discharged in less than 48 hours from his stroke onset and returned home to continue his recovery.
“I’m thankful someone saw the signs and didn’t hesitate,” Honeck said. “And I’m even more thankful that the people on the other end were this prepared.”
The novice golfer’s next steps post-stroke will include following up with his Sutter primary care doctor, who will help guide his next few weeks of care and will work with him to prevent future strokes.
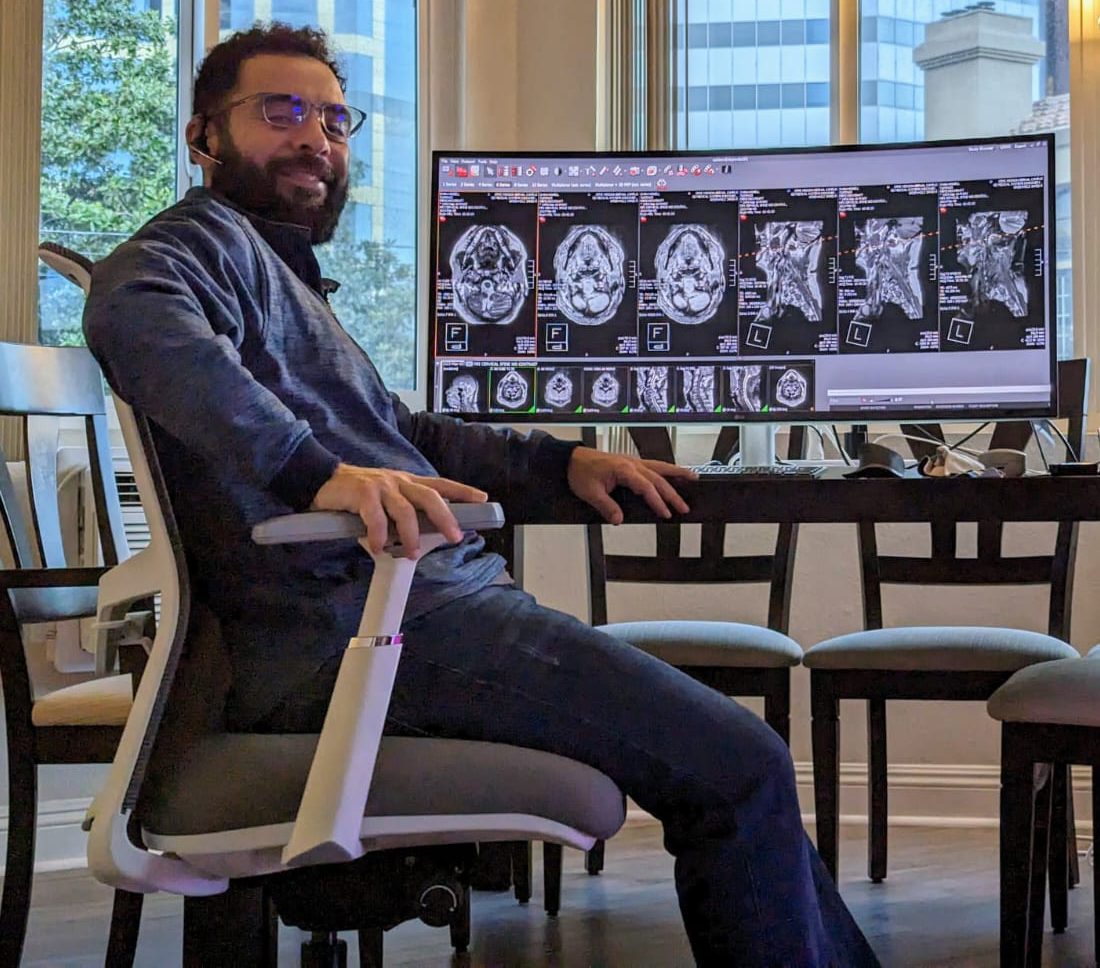
Vascular neurologist Dr. Mateo Calderon reviews a patient’s brain scans remotely as part of Sutter’s telestroke network.
Honeck’s story is a powerful reminder that stroke care is more than just fast action. It’s about well-rehearsed precision, planning, communication and teamwork, explains Dr. Barazangi. It’s why Sutter has invested in a fully integrated stroke response model across its hospitals, connecting local teams with stroke specialists within seconds.
Dr. Barazangi puts it simply, “We’ve designed our stroke care system to give every patient the best chance at life and recovery no matter where they enter the Sutter system. And it starts before they even reach the hospital.”
Recognize the Warning Signs of Stroke
In Honeck’s case, his journey began with his golf instructor smartly recognizing the signs of stroke.
Should a stroke occur, one important tool to help others and yourself is learning the BEFAST acronym:
Balance – Sudden loss of balance
Eyes – Sudden changes in vision
Face – One side of the face droops
Arms – Arm weakness
Speech – Slurred or hard-to-understand speech
Time – Call 911 immediately
When it comes to stroke, time saved is brain saved. And in Honeck’s case, it made all the difference. He was able to receive the right treatment, recover and return to work the following week.
“I’m feeling lucky,” he said. “Everyone moved so quickly and knew exactly what to do. But I also realize luck wouldn’t have mattered without such a well-prepared team.”
Bringing Clinical Trials to the Bedside
Although Honeck wasn’t eligible for a stroke trial, patients across Sutter’s advanced stroke network may have the opportunity to participate in clinical research, and sometimes while care is already in motion. Through rapid protocols, streamlined telemedicine consent and close coordination between hospitals, Sutter is able to offer access to promising new therapies without delaying critical treatment. It’s one more way the health system is bringing innovation directly to the bedside, even in the midst of an emergency.






