The race is on and the goal is clear. The U.S. needs new healthcare providers to replace the estimated 35% of the physician workforce that will reach retirement age in the next five years. Formal education alone isn’t going to fix the problem.
“It’s the postgraduate training — often done on the job, with a mentor — that can become a limiting factor,” says Dr. Robina Moen, internal medicine physician with Palo Alto Foundation Medical Group and its medical director for clinician teams. “You can’t enter the field of medicine with book-based learning alone. You need practical, hands-on clinical experience and lots of it.”
While medical education programs have increasingly made externships, fellowships and other forms of apprenticeship a requirement for degree completion, some forward-thinking healthcare employers have another approach. They are launching their own continuing education options for new hires. One such program, for recently graduated and newly hired advanced practice clinicians, is offered by PAFMG, part of the not-for-profit Sutter Health system.
A Serendipitous Start
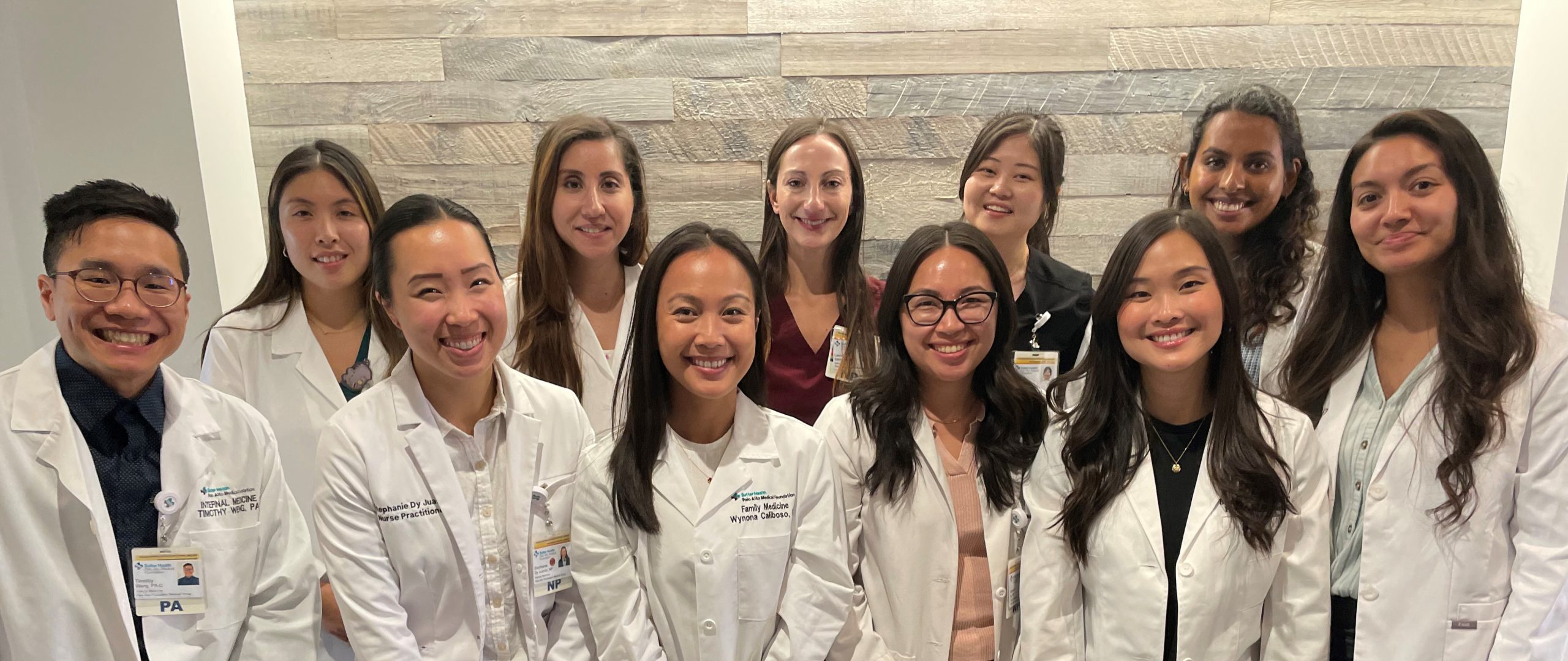
The inaugural cohort of providers in the LAUNCH program, which stands for Leading and Uplifting New Clinicians into Healthcare, consists of six nurse practitioners and seven physician assistants. The group started onboarding at PAFMG in mid-September and coincidentally started seeing patients on Sept. 25 — the same day that kicked off National Advanced Practice Clinician Week.
This annual observance is designed to honor the important group of clinicians known as Advanced Practice Clinicians, which includes physician assistants, nurse practitioners, certified nurse midwives, clinical nurse specialists and certified registered nurse anesthetists.
The observance also aims to raise awareness of the scope of duties these medical professionals can perform. “APCs are nationally certified and licensed to assess, diagnose, treat and manage illness, prescribe medications and perform clinical procedures,” says Surani Kwan who holds a doctorate in nursing practice and the title director for professional practice and nursing excellence at Sutter Health. “At Sutter Health, we rely on these professions as an integral part of our care teams,” Kwan continued.
More than 2,000 APCs practice at Sutter Health today, and Sutter has plans to attract, grow and retain more APCs in the years ahead. The LAUNCH program, which will have cohorts in the spring and fall each year, is one example of making that goal manifest.
Tonic for Transition Shock
Over the next three months, 13 newly hired APCs will receive additional training from PAFMG clinicians, designed to supplement their formal education. The program’s goal is to reduce “transition shock” – a phenomena where new medical providers can feel anxious or inexperienced in their roles, responsibilities or knowledge.
“We recruit nurse practitioners and physician assistants from highly diverse backgrounds, and naturally that comes with variable levels of experience in health care,” said Amy Bennett, director of advance practice clinicians for PAFMG and herself a nurse practitioner. “We want to offer proper preceptorship and coaching to establish a good knowledge base, and ultimately create a successful workplace.”
Tim Weng, a physician assistant in the inaugural LAUNCH program says he looks forward to the extra training he will receive. “I entered physician assistant school in September 2020, when COVID-transmission was a huge concern,” he recalls. “My clinical rotation in obstetrics was withdrawn and other placements were cut short, so the LAUNCH program is especially valuable for me and anyone who found themselves in a similar position during the protracted pandemic.”
Co-developed by Bennett and Dr. Moen, the program has five key features: a clinic with a physician onsite just to answer questions (they are not seeing patients), another clinic where preceptors emphasize – and exhibit – team-based care of patients, opportunities to shadow specialists, a peer mentorship and support group, and didactic presentations on the art of practicing medicine. The PAFMG providers who dedicate their time to LAUNCH training activities are compensated using philanthropic funds. These monies come courtesy of generous community donors who appreciate how a program like this can improve access to the high-quality, personalized care that Sutter is known for.
The breadth of topics and level of support is intentionally broad says Bennett, joking that the program covers “everything that wasn’t on your board exam.” Dr. Moen agrees, emphasizing that new APCs often need to learn the nuts and bolts of documentation in electronic medical records, for example, including how to code for services, how to request a specialist referral, and how to ensure follow-up and continuity when helping a patient manage chronic illness.
The duo say that the future of medicine will take a team-based approach, with physician and APCs working together, right from the start!