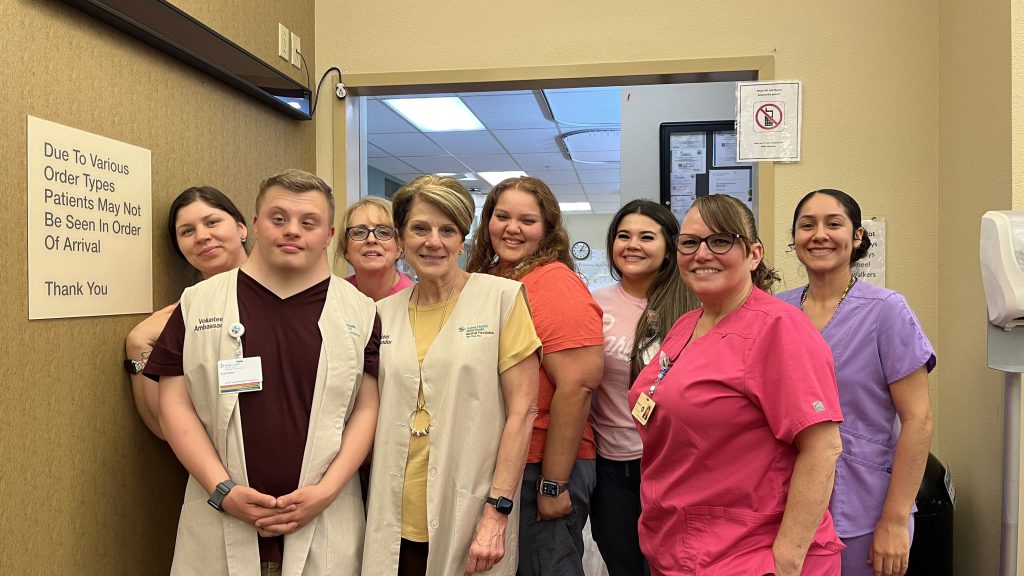
Tara Jasper’s breast cancer diagnosis brought clarity about genetic testing as a powerful cancer prevention strategy. She’s working with Sutter Health to spread awareness about its no-cost genetic testing & counseling program called GREAT.
Knowing your cancer risk can start by spitting in a tube? That’s right!
“The results,” says Tara Jasper, “might just save your life.”
Jasper is a 45-year-old wife, mother, pilot and gin distiller. The Healdsburg, Calif., resident is also passionate about raising awareness for genetic testing for breast, ovarian and other cancers.
“Fabulous technology already exists and we’re not taking advantage of it,” she says.
She is confident her work with Sutter Health to support the expansion of a genetic testing and counseling program will help accelerate catching people’s cancers earlier and preventing future cancer diagnoses.
Motivated out of frustration
Jasper is no stranger to hearing those dreaded words: You have cancer.
While she beat it, she acknowledges that if she’d had key genetic information sooner in life, she would have prevented her cancer entirely.
A 3D rendering of a DNA strand.
Jasper, whose mother passed away from breast cancer, asked her doctor in 2013 for a genetic test. She was denied because she did not meet the criteria based on existing guidelines. Also, at the time, an independent genetics test would have cost her thousands.
It was six years later in 2019 that she discovered a lump in her breast. Her doctor recommended a lumpectomy.
Before surgery, at the behest of a doctor-friend, Jasper sent away for a genetic testing kit.
“It arrived on my doorstep three days later and cost $200,” she says.
The results revealed that Jasper carries the BRCA2 gene mutation. She was floored!
Now, armed with this critical information about her genetic mutation, she opted for a double mastectomy.
What’s more confirmation, Jasper says, is that during the procedure, her surgeon found two more tumors that had never been seen in any scan due to her dense breast tissue. She credits the BRCA2 diagnosis with saving her life.
“Why aren’t more people doing this? They’re getting diagnosed with cancer and then they’re finding out afterwards they’ve got this genetic mutation,” she said. “That’s unacceptable.”
She adds, “If they can find out with this affordable test, then the option of avoiding cancer altogether is there.”
Astonished by the ease at which she ordered the test, its relative low cost, and how quickly she received her results, Jasper was motivated to help change the outcome for others.
“I was pissed off,” says a feisty Jasper. “I channeled that frustration for women and men everywhere, and Sutter made it possible for me to get involved.”
The launch of GREAT
Together, Jasper and Sutter Pacific Medical Foundation partnered on Gin & Genes, a fundraising effort to support Sutter’s Genetic Risk Evaluation and Testing (GREAT) Program. The program offers no-cost genetic testing for patients between the ages of 25-45 and with no personal history of cancer.
In many cases, health insurance plans will cover the costs of genetic testing when it is recommended by a patient’s doctor, but there may be instances where insurance policies or criteria make the requirements unnecessarily specific and difficult for the person to move forward.

Sharon Chan, manager of genetics for Sutter’s Palo Alto Medical Foundation
“Our goal is to personalize cancer screening for individuals who may have an increased risk for cancer,” says Sharon Chan, manager of genetics for Sutter’s Palo Alto Medical Foundation.
Chan oversees the GREAT Program, which is supported by 13 other genetic counselors across Sutter Health in Northern California.
“If you have a genetic mutation, your parents, children and siblings each have a 50% chance of having the same mutation,” says Chan. “Screening family members for known familial genetic variants gives those who test positive the opportunity to make informed decisions on prevention strategies.”
Chan likens it to playing offense with your health instead of defense.
“If it were up to me, everyone would get genetic testing,” she says.
In its first year, Sutter’s GREAT Program focused on laying the groundwork to educate the health system’s physicians about the benefits of genetic testing for patients. Sutter oncologists routinely refer patients for genetic testing and counseling with Chan’s team, but other physicians outside Sutter’s oncology specialty may not know these resources are available, so creating that awareness is key.
This year, the program’s second, the focus is on activation. It’s about getting the word out to the community so patients can access genetic testing and counseling services at Sutter.
Sutter’s GREAT Program uses a saliva-based genetics testing kit, no blood draw required. The materials are shipped to the patient’s home and mailed to Sutter’s lab partner. Once the results come back, in about three weeks, a Sutter genetics coordinator will get in touch with the patient and set up a tele-health appointment with a genetic counselor to review the results.

Sutter Health genetic counselors can help you decide if genetic testing is right for you.
Reviewing the results with patients is just as critical. Chan explains the counseling piece of the program is particularly important because people need to know what to do with the information they’re receiving.
“The results don’t mean much if there’s no counseling behind it,” she says.
“Depending on a person’s test result, they may qualify for increased health screenings. Patients can also talk with the counselor about other medical interventions and lifestyle modifications, like diet and exercise, that can be incorporated into their routines.”
Outdated guidelines need to change
The guidelines that qualify a person for a genetic test need to change, says Jasper. Currently, to get genetic test coverage, most insurances require a patient to have at least two family members who have breast or ovarian cancer.
The challenge is that many people don’t realize such tests exist or that they can order one if they do not qualify, albeit with a cost. Sutter’s GREAT Program is no-cost.
“It’s the invisible knowledge that genetic testing provides, which has the power to change futures,” says Jasper. She’s referring to her own daughter and the thousands each year who could one day be diagnosed with a preventable or more easily treatable breast or ovarian cancer had they had this knowledge.
“What you know now can help you be around longer,” Jasper says, “and that’s worth it. I know it will for sure save lives.”