Early lung cancer care just got remarkably faster.
Sutter Health’s California Pacific Medical Center (CPMC) is using a novel approach to diagnose and treat lung cancer in one surgery using the latest robotic technology.
Eliminated for patients are weeks of worry, repeat specialist visits, and separate surgical procedures.
The Assisted Single Anesthetic Procedure (ASAP) allows for multiple medical procedures to be completed back to back, condensing what was previously a multi-week affair of anxiety, anticipation, and logistics.
The new model represents a major paradigm shift in how doctors diagnose and treat suspected early-stage lung cancer.

Sutter Health’s California Pacific Medical Center (CPMC) Van Ness campus in San Francisco.
“CPMC is the first hospital in San Francisco to offer this streamlined approach with robotic-assisted bronchoscopy,” says Dr. Heba Ismail, an interventional pulmonologist who directs CPMC’s Lung Cancer Program.
Robotic-assisted bronchoscopy is cutting-edge technology that can detect lung cancer in its earliest stages when it is easier to treat and cure.
CPMC has completed nearly a dozen procedures with more planned, says Dr. Ismail.
“Patients come to CPMC from all over Northern California to be treated for their lung cancer,” says Dr. Jey Chung, an interventional pulmonologist at CPMC. “Providing multi-disciplinary, coordinated care and offering our patients an opportunity at diagnosis, staging and curative surgical treatment in one operative setting allows these individuals to move forward more rapidly with their cancer care and, most importantly, their lives.”

Dr. Heba Ismail navigates a patient’s lungs using robotic-assisted bronchoscopy. This innovative technology can detect lung cancer in its earliest stages when it is easier to treat and cure.
Prior to launching the ASAP model, when a patient was diagnosed with a suspicious nodule, they were referred to a pulmonologist for lung biopsy. If the nodule was confirmed to be cancerous, the patient would next be referred to a thoracic surgeon for further evaluation. If deemed a surgical candidate, he or she would then undergo another procedure on a separate day to remove the mass. On average, individuals wait up to two months from their diagnosis to receiving treatment.
The new approach at Sutter Health using the ASAP model significantly speeds this process.
“This single protocol is complete in about three to four hours—a stark contrast to the traditional approach necessitating three or more different procedures averaging two hours each, pre- and post-op protocols needed for each procedure, and the resources required for each,” says Dr. Ismail.
From weeks to hours, here’s how ASAP works
While the patient is under general anesthesia, CPMC’s ASAP team uses minimally invasive robotic-assisted bronchoscopy to navigate to the suspicious mass and obtain a biopsy. The tissue sample is then delivered to a pathologist who determines within 15 minutes if the diagnosis is cancer. If it is, the surgeon will proceed with sampling of the patient’s lymph nodes. The ASAP team will then use the same navigational route to mark the cancerous lesion for removal. Lastly, the patient who is still asleep, will have a second minimally invasive procedure (robotic or video-assisted thoracoscopic surgery / VATS) to remove the cancer.
The individual will be discharged 48-72 hours later.

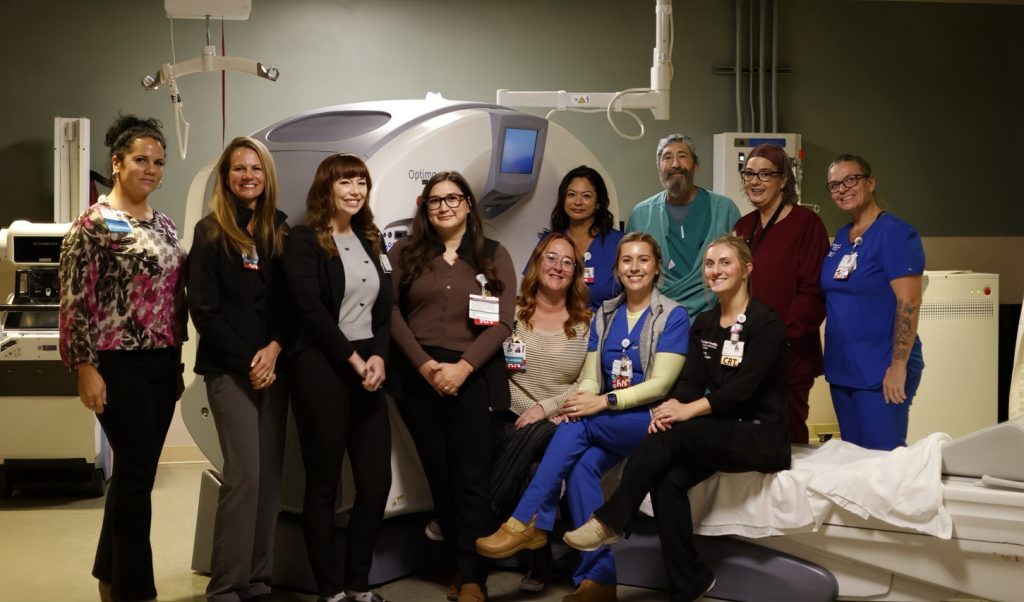
The ASAP surgical team at Sutter Health’s CPMC in San Francisco.
Cardiothoracic surgeon Dr. Peter Anastassiou, director of CPMC’s Thoracic Oncology Program, explains that the ASAP protocol requires coordination of services and counseling of patients regarding their options, procedures, and prognosis.
“Because of robotic localization (using robotic-assisted bronchoscopy), patients with very small tumors can undergo segment resections rather than lobectomy,” he says.
The result for patients potentially means earlier recovery, decreased complications, and shorter hospital stays.
Early-stage lung cancers have 5-year survival rates up to 90% but most are caught late, making this disease the No. 1 cause of cancer death.
Individuals aged 55 or older, and who are long-time smokers or former smokers, may be eligible for a lung cancer screening at Sutter Health.
For more information on Sutter’s ASAP program, call 415-600-6070.