If you or someone you know has a mental health need or is struggling emotionally, there are ways to get help. Call or text 988 to receive confidential support from a trained crisis counselor, 24 hours a day. In an emergency, call 911. The programs and services discussed thin this article are not a replacement for consultation with your healthcare provider.
The collaborative care model, described below, is designed to support patients who experience a broad range of behavioral health disorders, including mild to moderate anxiety, depression, attention-deficit/hyperactivity disorder, bipolar disorder, or post-traumatic stress disorder. In this model your primary care provider stays at the center of your care—coordinating closely with a behavioral health care manager and consulting psychiatrist behind the scenes, so your physical and mental health can be cared for together.
When it comes to mental health and well-being support, asking for help can feel daunting. Yet that initial step is often the start of healing—and it can uncover resources you never knew existed. Over the past year, patients and providers at Sutter Health have experienced this type of unexpected help firsthand. Read how digitally enabled support has improved patient access to behavioral health care, lightened clinicians’ mental load, and is poised to offer greater emotional connection in the new year.
Collaborative Care
‘Fast’ and ‘easy’ aren’t words commonly used to describe mental health care, but Sutter’s adoption of the Collaborative Care (CoCM) imodel is changing that. Collaborative Care is a team-based approach in which the primary care provider treats a patient’s mental health needs, like depression or anxiety, with the support of a therapist and psychiatric consultant. Promoting upstream behavioral health, it includes routine mental health screening, tracking symptom improvement and evidence-based interventions like cognitive behavioral therapy.
Since January 2025, more than 4,800 Sutter patients have been referred to CoCM, coordinated by Concert Health. Operating as a first step in the behavioral health care service continuum, Concert uses its digital savvy to engage with patients in behavioral health care that works for them.
First, Concert integrates with Sutter’s electronic medical record, enabling secure referrals and real-time updates. 
- 7,579: Total referrals so far.
- 673 Sutter primary care providers can refer today.
- 75% have made at least one referral.
17 cities: Lakeport, Crescent City, Palo Alto, Daly City, Fremont, Los Altos, Dublin, Calif. and others are served today.
Once a referral is received, a member from the Concert team calls the patient to initiate care, instead of the other way around.
- 4 days: Average time from referral to first call.
 On that call, patients are enrolled and scheduled for a phone or video visit with a Concert behavioral health care manager to establish a care plan.
On that call, patients are enrolled and scheduled for a phone or video visit with a Concert behavioral health care manager to establish a care plan.
- 4,886 Sutter patients have enrolled with Concert so far.
- 6 days: Average time from enrollment to first virtual visit — compared to 43 days, the National median wait time for a telepsychiatry appointment without Concert Health.

Care continues through regular virtual visits with a Concert care manager.
- 55% of patients improved after 90 days (5-point or greater symptom drop)
- 95% of patients surveyed answered “yes” to the statement “My Concert Health care manager helps me feel better.”
Your treatment plan, progress and any changes are shared with your primary care provider for a holistic team approach. Concert care managers consult on a weekly basis with psychiatrists to optimize care.
These impressive numbers, which reflect services through October 31, 2025, tell only part of the story. Behind the data are real people whose lives are changed because they got help faster and more conveniently through the collaborative care model delivered by Sutter and Concert Health.
Take Tayla, a 12-year-old from Lakeport, Calif.—a rural community where access to mental health care is scarce. Tayla had been struggling with anxiety and depression and when her parents tried to get her help, they encountered long waitlists and found that services didn’t fit Tayla’s needs or schedule.
When Tayla’s pediatrician referred her to Concert, everything shifted. Within days, Tayla met with a therapist virtually and began building a plan for healing. As her mom, Brittani shared, “It almost felt too good to be true; Tayla opened up right away (because) she felt seen and safe.” Stories like Tayla’s remind us what’s possible when barriers disappear and care meets people where they are.
Virtual Scribe
With almost half of U.S. physicians reporting symptoms of burnout, prioritizing clinician well-being has never been more critical. One place to start: reduce the clerical tasks that keep providers working late, logging in from home, and missing time with their families.
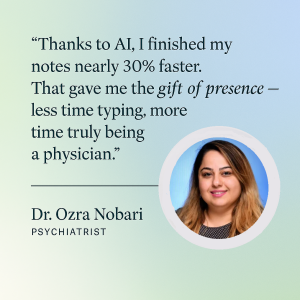
One of the most time-consuming of these administrative burdens is “charting” or documenting every patient interaction in the electronic health record. While these notes are necessary, one company has developed a tool that lets AI handle most of the work, saving clinicians time and, as Sutter has found, decreasing their mental fatigue too.
In early April 2024, Sutter began piloting software from Abridge, Inc., which uses ambient listening to transcribe a draft clinical note, in real time, from the conversation had during a medical encounter. Sutter tested and refined the tool and simultaneously studied its effects on the level of cognitive demand or memory burden that clinicians felt during their workday.
Through survey questions, Sutter researchers asked providers about the level of mental fatigue they felt before and after trying Abridge. They found that a statistically significant number of respondents ‘agreed’ or ‘strongly agreed’ that the tool reduced their cognitive burden, specifically:
- 52% responded they felt less hurried or rushed to complete notes when they used the tool.
- 48% responded that the mental demand associated with notes was less after using the tool.
- 41% responded that the difficulty they felt in completing notes fell after using the tool.
These three questions, taken together and asked of a larger survey sample, found that 49% of clinicians overall reported less cognitive load when using Abridge for notetaking.
Today, more than 3,200 Sutter-aligned physicians and advanced practice clinicians are using Abridge across multiple settings of care, including: outpatient medical offices (both specialty and primary care), hospital emergency departments, and Sutter Center for Psychiatry (SCP) – a psychiatric hospital offering Inpatient, partial hospitalization and intensive outpatient programs for adults, teens and children.
The Chief Medical Executive of SCP, Dr. Ozra Nobari, recently shared her experience with Abridge, highlighting how she could focus on listening and had more mental space to think and process the information her patient shared when she wasn’t taking notes during the visit.
“Due to the nature of the care provided, psychiatrists spend long hours documenting their observations. This time was different. I turned on my AI note taker and forgot about documentation. Finally, I was fully present. I was able to closely monitor my patient’s progress, adjust the dose of medicine, fine-tune his behavioral activation plan, make numerous calls with his family to both learn and update, and coordinate the delicate dance with our amazing nursing team, pharmacy team and psychiatry technicians. The result? A boy who hadn’t moved or spoken just days earlier, completely disconnected from the world, took a step toward healing — and I watched hope spark in his family and in my team’s eyes. ~ Dr. Ozra Nobari
Text-based Support
If you’ve ever received a supportive text message that tlifted your spirits, you’re not alone. A simple reminder that someone is thinking of you can have a meaningful impact on emotional well-being.
This is the premise behind Caring Contacts, a program that sends brief, supportive messages to teens and young adults who have been treated for suicidal thoughts or behaviors. Designed to remind individuals that they are cared for, the program helps to bridge the gap in care after a patient has been discharged from a hospital emergency department or behavioral health unit.
Sutter will begin piloting Caring Contacts next year, with messages that have been tested with – and improved by – a diverse group of young people.
- 19 messages: sent the day after discharge, then weekly for 8 weeks, monthly for the remaining 9 months and on the patient’s birthday
- 13-26 year olds: will receive messages and – if they consent – their parent or caregiver can receive them, too.
- 290+ young people: provided feedback and suggestions to refine the text and emojis that Sutter will use in each message.
“Sending a young person a supportive, caring text that encourages self-compassion during times of emotional distress has been shown to reduce the risk of suicidal behaviors,” said Tam Nguyen, clinical psychologist and behavioral health service line executive at Sutter Health. “I am excited to start offering this evidence-based service to Sutter patients in 2026!”