Sutter neurosurgeon Dr. Matthew MacDougall pictured during the VNS implant procedure at Sutter’s CPMC. The device aims to restore functionality to Kendall’s hand and arm following a stroke.
Vagus nerves, the longest cranial nerves in the body, run from the brain to the large intestine. There are two nerves, one on each side of the body, that wind through the medulla oblongata and extend down the neck, chest, heart, lungs, abdomen and digestive tract. They act as a busy information superhighway, connecting the brain to many important organs and helping control automatic body functions like heartbeat and digestion.
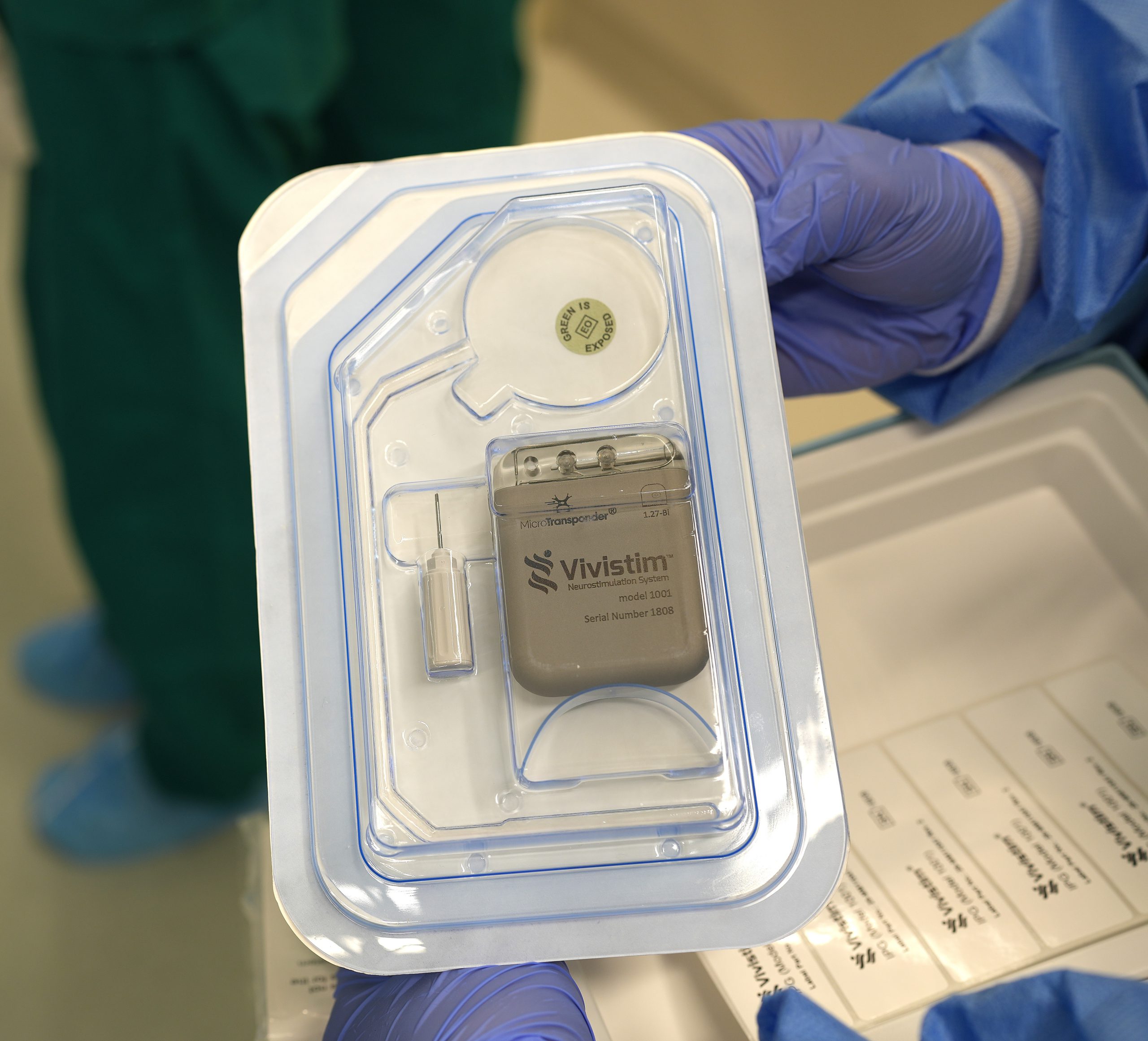
The palm-size VNS device, about the size of a domino and measuring 48 millimeters wide, 62 millimeters tall and 12 millimeters thick, is surgically placed in the patient’s neck and chest. A coil connected to the device is wrapped around the nerve and secured to deliver electrical impulses during treatment sessions.
To place the VNS Vivistim® device, manufactured by MicroTransponder Inc., Dr. MacDougall created a 1-inch incision on the left side of Kendall’s neck and dissected down to the vagus nerve where the coil was secured. Then, through a 3-inch incision on the left side of his chest, the device was carefully implanted.
Pairing VNS with Rehab
To help speed Kendall’s recovery and minimize the risk of complications, care teams at Sutter’s Ray Dolby Brain Health Center will provide comprehensive, continuous follow-up care during and after rehabilitation therapy.
Patients like Kendall are treated with the same initial rehabilitation protocol. Once cleared by their neurologist, they can begin a six-week home rehab program, plus in-person occupational or physical therapy sessions. For at-home therapy, patients can swipe a self-activation magnet across their chest and go about their everyday activities to build arm and hand strength. After six weeks, patients will continue with at-home therapy indefinitely with ongoing support from their care team.
“The goal of post-stroke VNS with rehabilitation is for the patient to stimulate their device during daily activities,” says Dr. Hal Fisk, manager of outpatient rehabilitation at CPMC. “This is crucial to regaining their independence and improving their long-term hand and arm function after a stroke.”
The neurology and neurosurgery teams at CPMC will work closely with the rehabilitation team to ensure people like Kendall can easily schedule therapy sessions post-surgery. Additionally, further studies are planned to seamlessly continue treatment for Kendall in his home, in collaboration with the MicroTransponder Inc. team.
“For patients facing the uncertainty of lasting upper extremity weakness from stroke, this novel approach offers a chance of meaningful, long-lasting improvement in hand and arm functioning,” says Dr. Momii. “It also highlights the brain’s neuroplasticity and its ability to adapt to changes. Through a multidisciplinary model of care, we at Sutter aim not only to improve function after stroke, but to restore hope, recognizing that rehabilitation is as much about the person as it is about the pathology.”

Mild electrical stimulation of the vagus nerve activates the parts of the brain that are important for motor learning.
Advancing the Future of Post-Stroke Mobility
Stroke researchers at Sutter are also looking at the ability of VNS to address cognitive impairment, such as speech disorders, and learn how the procedure may inform care for individuals with other neurologic illnesses.
“By integrating VNS into our comprehensive stroke care program alongside the Ray Dolby Brain Health Center and Sutter Davies Rehab Program, Sutter is at the forefront of advancing stroke recovery options using a multidisciplinary approach, even for patients in the chronic or early phases of rehabilitation therapy,” says Dr. Momii. “This is a game changer in the high-quality stroke and rehabilitation care we are proud to offer our patients.”
Do you or a loved one need rehabilitation services after a stroke? Learn more to be connected to a Sutter stroke specialist for assessment.