Life can change in an instant. When a stroke turns a normal day into a health emergency needing immediate and specialized care, every second counts to help prevent lifelong disability and even death. With 17 Joint Commission-certified stroke centers in Northern California, Sutter Health stroke specialists and care teams provide advanced care to more than 6,000 stroke patients each year thanks to a steadfast focus on clinical excellence.
“Our teams at Sutter are continually focused on advancing the already high-quality stroke services we offer by implementing the latest technologies for rapid stroke assessments and treatment,” says Dr. Shawn Kile, neurologist and neuroscience service line chair at Sutter Health.
“This high level of coordinated stroke care across our network is what leads to the very best outcomes for our patients with these brain emergencies.”
Using Technology for Quick Diagnoses and Treatment
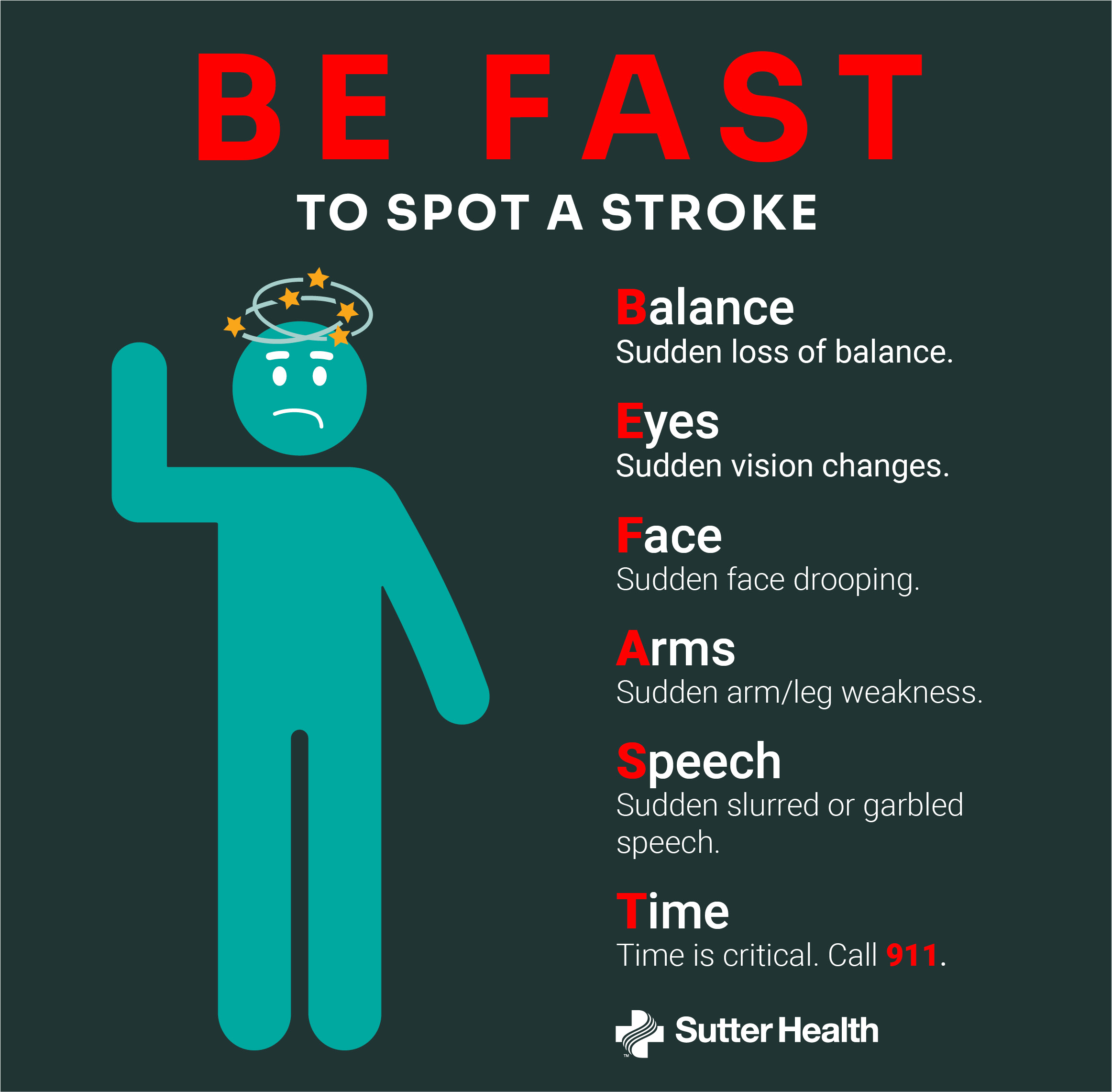
It’s crucial to BE FAST to spot a stroke. Sutter’s innovative approach to stroke care leverages technology to quickly diagnose and triage patients, helping reduce stroke-related disabilities and death.
Sutter’s Telestroke Program, one of the largest in Northern California, enables a specialized team of stroke specialists and staff to remotely deliver 24/7 stroke care. This level of swift, high-quality and coordinated care can prove to be critical, especially for people in small or rural communities with limited access.

The Mobile Stroke Unit is staffed with a specially trained stroke team and includes a CT scanner for quick diagnosis.
Another way Sutter delivers prompt stroke care to its communities is through its Mobile Stroke Unit (MSU). This specialty ambulance has advanced technologies and stroke specialists on board, enabling rapid CT imaging and diagnosis during patient transfer to the emergency department.
Sutter stroke centers and hospitals that are telestroke sites leverage innovative technologies like RapidAI, whereby Sutter stroke specialists and care team members can receive imaging results before a patient has been transferred to the hospital. This means doctors can quickly diagnose, triage and quickly administer care while running against the clock.
Practicing and Studying the Latest Medicines
TNK, a blood clot-dissolving drug, delivers lifesaving treatment to stroke patients. The quick-acting and easily administered medication “busts” the clot, restoring the flow of oxygen and helping prevent long-term brain damage and lifelong disabilities. In some cases, patients who receive TNK or other clot-dissolving drugs don’t need more invasive treatment like thrombectomy—a surgical procedure that removes the clot blocking an artery.
“When thrombectomy is required, it’s important that care is delivered quickly and skillfully, like any stroke treatment, to preserve as much brain tissue as possible. At Sutter, the advanced stroke center designations—where approximately 450 thrombectomies are performed annually—continue to grow,” says Dr. Nobl Barazangi, Sutter West Bay Medical Group physician practicing at California Pacific Medical Center and Mills-Peninsula Medical Center, and chief of stroke for Sutter’s neuroscience service line.
In addition to using cutting-edge treatments and performing highly specialized stroke surgeries, Sutter participates in clinical research to continue advancing the highest-quality stroke care. For example, Sutter is participating in the U.S. National Institutes of Health StrokeNet FASTEST clinical trial along with 100 hospitals and 15 MSUs. The study, still open to enrollment, is evaluating a drug used to treat hemophilia to determine if a blood clotting factor can stop the progression of an acute hemorrhagic stroke.
Research at Sutter is also helping inform cost-effective care so patients and the health system benefit from smart health care utilization. The BEST-MSU clinical trial showed patients treated by MSU reported better average quality of life and spent nearly two weeks more at home compared to those who received standard care by emergency medical services. The study also showed MSUs were increasingly cost-effective as the number of treated patients increased.
Sutter participated in the ESCAPE-MeVO clinical trial that showed endovascular treatment for acute ischemic stroke due to medium-vessel occlusion within 12 hours did not lead to better outcomes at 90 days than usual care, paving the way for further study and trials.
Training the Next Generation of Stroke Specialists
By building a nationally recognized Graduate Medical Education program, Sutter is training the next generation of leading physicians to deliver highly specialized care in specialty areas of medicine like neuroscience. Sutter Roseville Medical Center recently received national accreditation for a neurology residency program.
The program will welcome 12 residents in July 2026, continuing the community-based approach to care and strengthening the physician workforce. Resident physicians will have the opportunity to train with specialists at the top of their field, further positioning Sutter as a leader in the care of stroke and other neurologic illnesses.
“At Sutter, we’re continually finding new ways to best train physicians to lead, advance care through research and ask and help answer the clinical questions that shape the future of medicine,” says Dr. Barazangi.
For more information about Sutter’s Stroke and Neurovascular Care, visit https://www.sutterhealth.org/services/stroke-and-neurovascular-care