Artificial intelligence advancements have come roaring back to life. From chatbots to image generators, content creation and conveniences abound for consumers. But what about the ways it can potentially have a more profound impact—like for one’s healthcare needs?
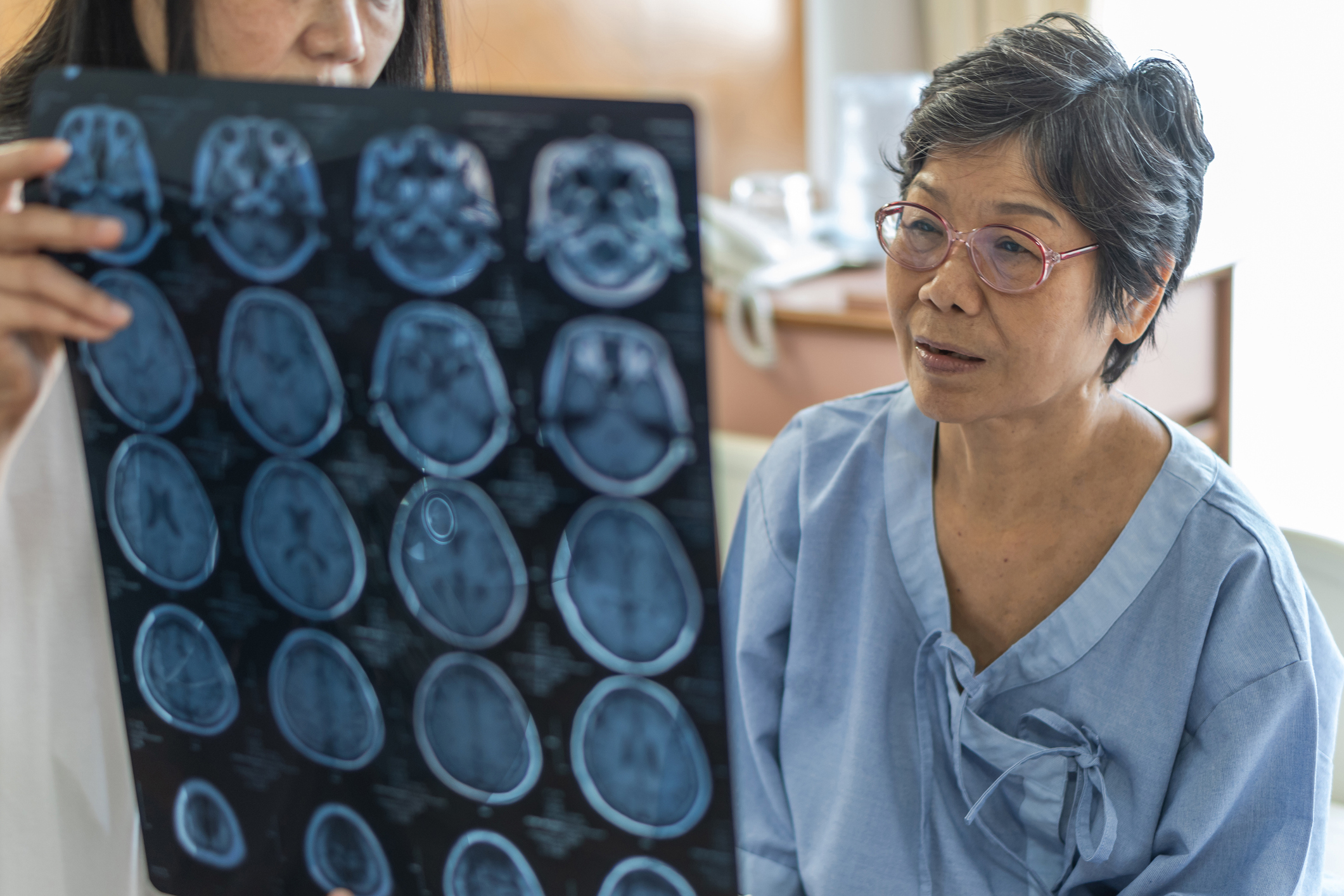
A novel approach that pairs AI with advanced imaging and mobile applications is helping propel stroke care with a new future. It’s one where emergency medicine and stroke specialists have the tools and clinical data they need—(even on a smartphone!)— to help doctors more quickly diagnose stroke and plan the course of treatment.
Northern California’s Sutter Health has collaborated with San Mateo, Calif.-based neurovascular technology developer RapidAI to usher this approach into stroke care across its integrated, not-for-profit system. Sutter is the only healthcare system in Northern California using the full portfolio of RapidAI applications.
“The use of AI-based imaging has the potential to save lives and improve outcomes for the millions of people who suffer from stroke globally each year,” says Dr. Manoj Mittal, medical director of Stroke & Neurocritical Care for Sutter Health’s Valley Area. “Patients who experience a severe, acute ischemic stroke may be transferred to one of our specialty hospitals for emergency care with thrombectomy to restore blood and oxygen flow to the brain. With the RapidAI software we can see images of the clot ‘on the fly’ as patients are transferred to the hospital.”
AI-based imaging with RapidAI: How it works
1. The RapidAI platform, available on a smartphone or other mobile device, helps stroke specialists quickly identify large blood vessel clots by automatically processing CT scans and delivering clear, easy-to-interpret CT images.
2. Results are delivered through the RapidAI mobile application and by email to stroke team members at the hospital and its emergency department in three minutes or less—helping doctors more quickly and accurately diagnose stroke and plan urgent treatment. So patients are more likely to recover without stroke-related disability and less likely to need follow-up procedures.
Learn about other advancements in stroke care at Sutter Health including novel clot-busting drugs and a Mobile Stroke Unit
“AI is particularly valuable in emergency medicine and stroke care because of the speed at which these treatment and triage decisions need to be made. It’s exciting to see stroke patients who have benefited from this approach and are alive and healthy today because of it,” says Dr. Mittal. “The teamwork of Sutter’s clinical neuroscience service line, its Stroke Operating Committee and critical partners continues to bring our patients new, lifesaving treatments and technologies that exemplify the power and impact of our coordinated approach to delivering high-quality, safe and innovative care.”
A stroke is a life-threatening emergency condition where every second counts. If you or someone with you has symptoms of a stroke, you need to IMMEDIATELY call 911 (or your local emergency services number).
The longer it takes to receive care, the more likely a stroke will cause permanent brain damage or death.
To recognize the warning signs of a stroke, remember to think FAST:
F is for face. Ask the person to smile. Look for a droop on one or both sides of their face, which is a sign of muscle weakness or paralysis.
A is for arm. A person having a stroke often has muscle weakness on one side. Ask them to raise their arms. If they have one-sided weakness (and didn’t have it before), one arm will stay higher while the other will sag and drop downward.
S is for speech. Strokes often cause a person to lose their ability to speak. They might slur their speech or have trouble choosing the right words.
T is for time. Time is critical, so don’t wait to get help! If possible, look at your watch or a clock and remember when symptoms start. Telling a healthcare provider when symptoms started can help the provider know what treatment options are best for you.