(Last updated Dec. 24, 2020)
In the biggest boost in the fight against the coronavirus, the first COVID-19 vaccine was authorized Friday by the U.S. Federal Drug Administration. State governments are now expected to authorize its use and begin getting it to those on the front lines and to high-risk individuals. How does it work? Here’s how vaccines help could protect a person from COVID-19.
One function of the human immune system is to inhibit viruses, and prevent them from causing illness. The body has two types of immune response to accomplish this function: innate immunity, which starts within hours of an infection, and adaptive immunity, which develops over days and weeks.
A virus causes an illness by infecting cells in the body and taking control of their genetic material. The virus then instructs these infected cells to reproduce the virus’s genetic code and replicate more viral “soldiers” that fight against our immune system.
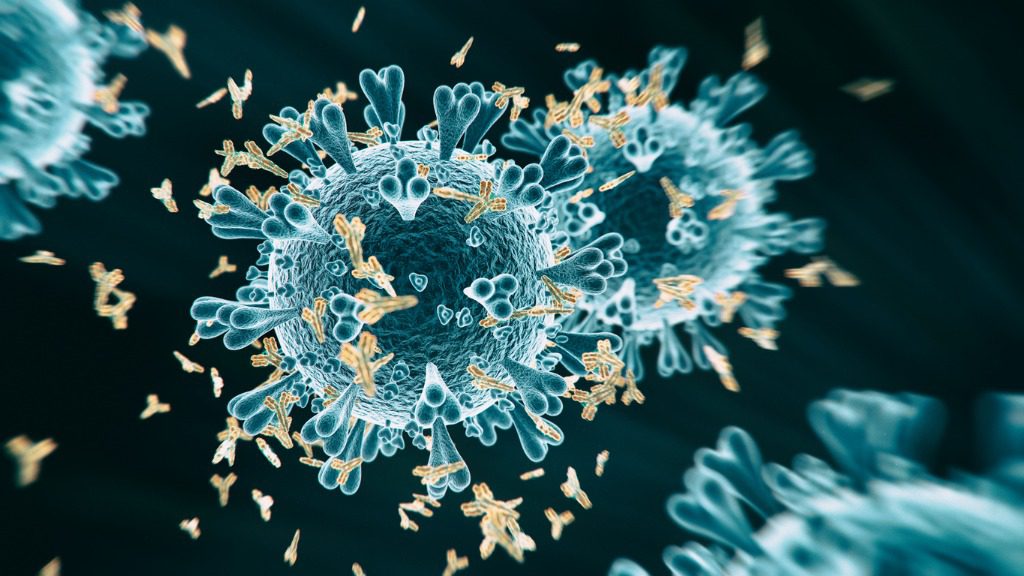
The body’s adaptive immune response consists of two types of white blood cells—called T and B cells—that can detect “signals” specific to the virus and assemble a targeted response to it.
T cells identify and kill cells infected by a virus. B cells make antibodies—a kind of protein that blocks viral material from entering our cells and prevents the virus from reproducing.
In case the body may need to fight the same virus again, the body stores T and B cells that helped eliminate the original infection. These “memory cells” help provide us with long-term immunity. How long is long-term? Antibodies produced in response to a common, seasonal virus last for approximately one year. But the antibodies generated in response to a measles infection, for example, can provide lifelong protection.
The human immune system and vaccines
Vaccines provide immunity, or protection against a disease without causing the illness. They are made using killed or weakened versions—called antigens—of the disease-causing virus. For some vaccines, genetic engineering is used to make the antigens included in the vaccine.
If you’re administered a vaccine to prevent viral infection, your immune system responds to the vaccine in the same way it would if exposed to the actual virus, by:
- Recognizing the proteins and other components of the vaccine as foreign;
- Making antibodies to “attack” the vaccine, as if it were the actual virus, and;
- Remembering the foreign invader and how to destroy it. This response means if you are exposed to the disease-causing virus again, your immune system can intervene before you get sick.
The science on COVID-19 vaccines
Vaccines typically require years of research and testing before reaching the marketplace or clinic. Scientists and medical researchers stepped up their game early in the pandemic to produce safe and effective immunizations quicker than usual. Each of the COVID-19 vaccines being tested use a different method to “attack” the virus and engage the immune system to fight infection. However, there are a few common approaches being studied in clinical trials:
- mRNA vaccines use one or more of the COVID-19 virus’s genes to provoke an immune response, using genetic material called messenger RNA (mRNA). COVID-19 vaccines that use mRNA work with the body’s natural defenses to safely develop protection (or, immunity) to the virus. The mRNA from a COVID-19 vaccine does not enter the nucleus of a vaccine recipient’s cell, which is where human DNA is stored. This means the mRNA does not affect, alter or interact with our DNA in any way. Both vaccines that were approved this month for emergency use in the U.S. are mRNA vaccines.
- Repurposed vaccines rely on vaccines already being used to protect humans against other diseases (e.g., tuberculosis) that may also be effective in protecting against COVID-19.
- Viral vector vaccines use a virus to deliver COVID-19 genes into cells and provoke an immune response. These vaccines typically use viruses that infect animals such as chimpanzees or monkeys to act as the “carrier” that prompts an immune response against COVID-19 in humans.
- Whole-virus vaccines use a weakened or inactivated version of COVID-19 to spark an immune response.
- Protein-based vaccines use a COVID-19 protein or its pieces to invoke an immune response against the virus.
Curious about other research at Sutter? Learn more.
References:
- World Health Organization. Accessed Aug. 11, 2020.
- The race for coronavirus vaccines: a graphical guide. Nature news feature, April 2020.