Like many women who receive a diagnosis of breast cancer, Michelle Goldsmith, was overwhelmed when her biopsy showed breast cancer. She had so many questions about her diagnosis and knew that difficult decisions lay ahead. She knew she needed to make a battery of appointments and ultimately visit oncologists and other specialists located in different locations.
As Goldsmith was beginning to make plans, a friend told her about the Multidisciplinary Breast Cancer Clinic that had just been launched by breast cancer specialists at Sutter East Bay Medical Foundation. Goldsmith made one phone call to a nurse navigator, and that set off a process that she now calls “life changing.”

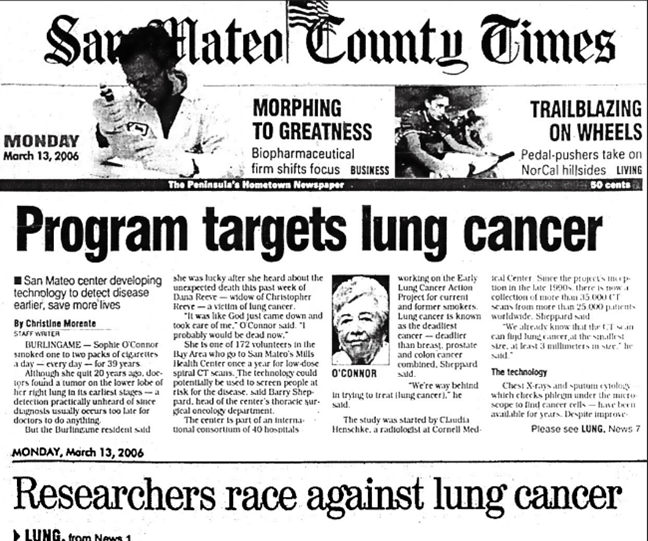
Michelle and Joe Goldsmith
The nurse navigator helped her plan the various tests and scans. The novel part of the process is that, once Goldsmith had the appropriate scans, all the oncologists and specialists met together in one pre-clinic conference call to go over her history and records to determine her best treatment for a cure.
Immediately after the call, Goldsmith was able to schedule a comprehensive team consultation with her breast surgeon in-person as well as virtual consultations with her medical oncologist and radiation oncologist.
After the two-and-a-half-hour appointment, Goldsmith left the office having met with her entire treatment team and with a one-page summary detailing her diagnosis, stage, and course of treatment. And because of the convenience of telemedicine video visits, Goldsmith could meet with all the specialists in one office, rather than seeing each one at a different time in a different location.
“It made all the difference in the world,” Goldsmith said of the multidisciplinary approach. “As a patient you feel so supported. It made me feel good that they had all agreed on a course of action, it wasn’t just one person’s opinion. And then you could see the oncologists face to face, and ask them as many questions as you wanted.”
“Part of it is looking at a way to have a much more streamlined approach for the patient,” explains Dr. Kwan-Feinberg. “With breast cancer, the treatment is always multidisciplinary so it makes sense for the patient to have one visit that is multidisciplinary and involves a team approach. From the patient’s perspective, I wanted each patient to have the best experience that would reduce the anxiety and fear that comes with a breast cancer diagnosis by answering all questions and having a treatment plan in one day.”
Dr. Consorti says a benefit is that the clinic helps coordinate the communication between different oncologists and specialists, and it is a convenient way for the patient to be able to speak to members of the team in one place, at the same time.
“Everyone is communicating in one fell swoop and is on the same page,” Dr. Consorti said, referring to the pre-clinic conference. “For the patient, it lays out their plan so they know what their care will entail.”
The two surgeons say it was a perfect time to start a patient-friendly, multidisciplinary program in part because of Sutter Health’s increasing capabilities in telehealth. After the patient meets with a breast cancer surgeon in person, an iPad is rolled into the office, and the patient meets via video visit with a medical oncologist and a radiation oncologist who are in other locations. And the program can be managed at a time when the number of in-person, office visits have been spread out to reduce possible exposure to COVID-19.
“The patient doesn’t go from office to office on different days so it minimizes exposure for patients and staff, and we have implemented deep cleaning procedures in the clinic,” Dr. Kwan-Feinberg said.
The pre-clinic virtual meetings are usually about 45 minutes long and include the breast surgeon, the medical oncologist, the radiation oncologist, the nurse navigator, the medical assistants and the surgery scheduler. Depending on the case, other clinicians are involved such as the pathologist, a geneticist and a lymphedema prevention specialist.
In addition to coming up with the best medical treatment, the plan that is given to the patient can be personalized, taking into account any relevant social issues or personal preferences. For instance, if a woman has children, there may be a list of child care resources. And, Dr. Kwan-Feinberg recalls that in one case the team learned that a patient was interested in herbal medicine so they included a referral in her plan to a physician who specializes in integrative or holistic treatments.
“My patients have been saying, ‘this is so great, I have a team taking care of me,’ ” said Dr. Kwan-Feinberg.