Ben Moseley, a healthy 13-year-old, is known for speed and agility on the basketball court. But in August 2022 an alarming spread of bacterial infection in his body stopped him in his tracks and jeopardized his life.

Ben Moseley, age 13
“It was truly frightening to see how quickly Ben’s health deteriorated without an easily recognizable cause,” says the teen’s mom, Sara.
She took her son to the emergency department at Novato Community Hospital, part of the Sutter Health system, after he began experiencing nausea, vomiting, rapid heart rate and confusion. Ben’s doctors administered fluids and ran multiple blood tests, which showed signs of acute kidney injury.
When Ben’s blood pressure continued to decrease, other symptoms worsened, and he became increasingly agitated and “just not himself,” he was transferred for specialty care to the pediatric ICU at Sutter’s California Pacific Medical Center in San Francisco. There, doctors gave Ben antibiotics and worked to restore his vital signs and prevent permanent damage to his kidneys, liver and brain.
A nurse caring for Ben at CPMC found a scab on Ben’s elbow that had new surrounding redness.
The culprit? A staphylococcus aureus bacterial infection that spread from Ben’s skin to his bloodstream, causing sepsis — a serious and potentially fatal condition that occurs when the body’s response to an infection damages its own tissues.
“It felt like my body was on fire inside and I couldn’t stop the flames,” reflects Ben.

Ben Moseley lays in a hospital bed as he battles sepsis, a serious and potentially fatal condition that occurs when the body’s response to an infection damages its own tissues.
Sepsis is a leading cause of in-hospital deaths and is optimally treated as swiftly as possible — making early detection crucial.
More than 18 American children die from sepsis every day, a number greater than deaths from pediatric cancers.
“Early identification of pediatric sepsis is particularly complex due to the variability of ages, weights and symptoms in infants and children,” says Dr. Erika Wong, a pediatric critical care doctor at CPMC. “For example, a common early sign of sepsis in an adult is low blood pressure, but in an infant or child this is a late sign and often means the child is already critically ill. I’m proud of Sutter’s use of screening tools, such as PEWS (pediatric early warning score), and other initiatives implemented across our network that are helping reduce the likelihood of missing the early signs of pediatric sepsis.”
After three days in the pediatric ICU, Ben’s blood pressure and heart rate stabilized and his mental state normalized. Doctors and nurses continued to monitor his condition, and after a full week in the hospital Ben returned home “good as new,” says Sara.
Dr. Wong encourages parents to know the signs of sepsis in children:
- Higher or lower body temperature than normal
- Bluish or very pale skin
- Lethargy or difficulty awaking
- Decrease or absence of urination
- In infants: not drinking or feeding
Act fast: Sepsis is a common, serious complication of an infection that requires urgent attention and fast treatment.
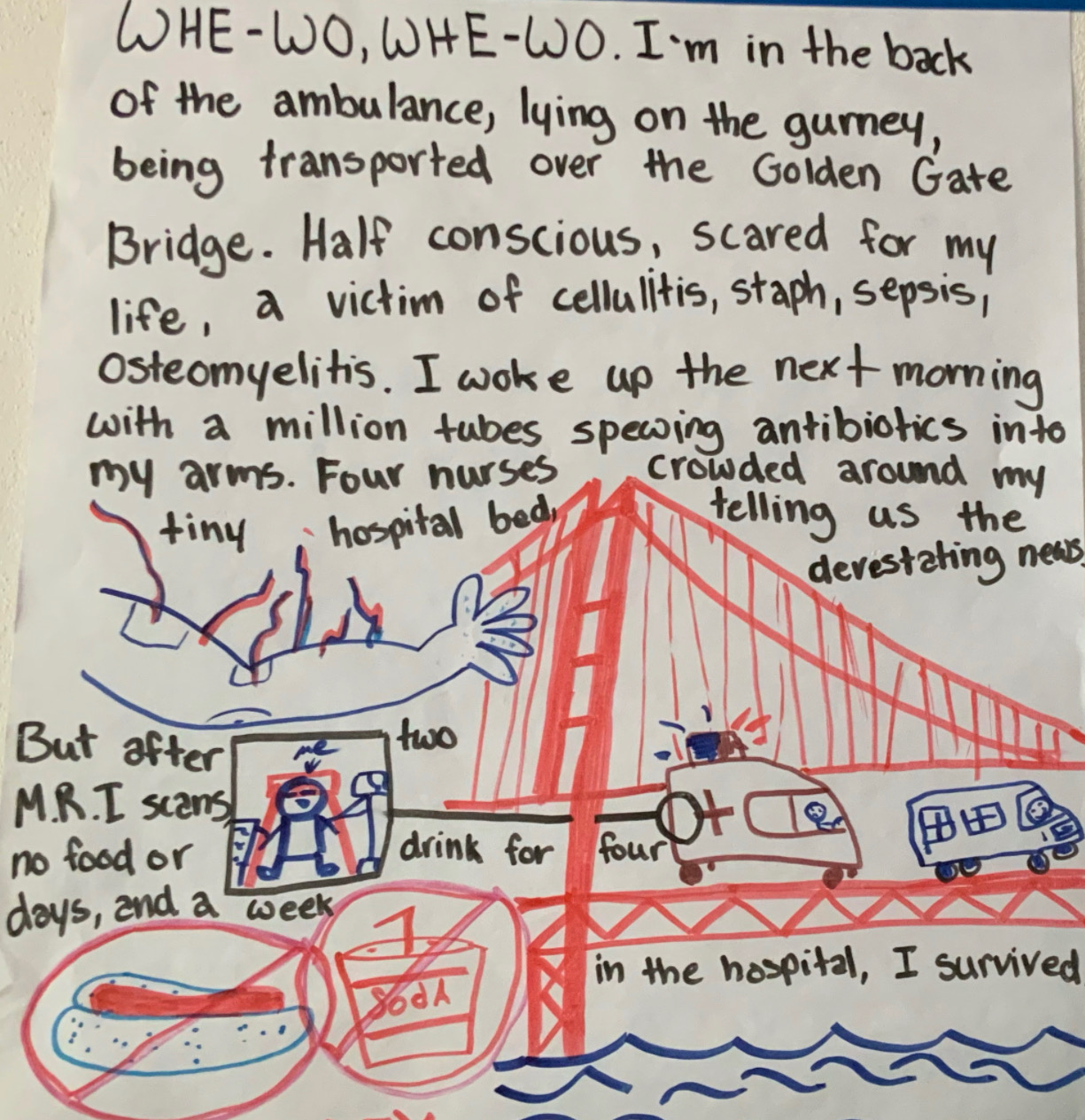
Ben’s illustration of what sepsis was like.
Note: This content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website





