Professional development is central to nurses’ lifelong learning and keeps their knowledge and skills up to date
Summer is winding down, but registered nurses at one San Francisco medical center are only now heading off to camp. More than 800 RNs at Sutter’s California Pacific Medical Center are participating in the hospital’s Competency Camp this June through November.
“The goal is to validate nurses’ knowledge while also sharpening their skills and clinical thinking,” says Delynn Peltz, CPMC’s director of nursing practice and quality, and the camp’s creator.
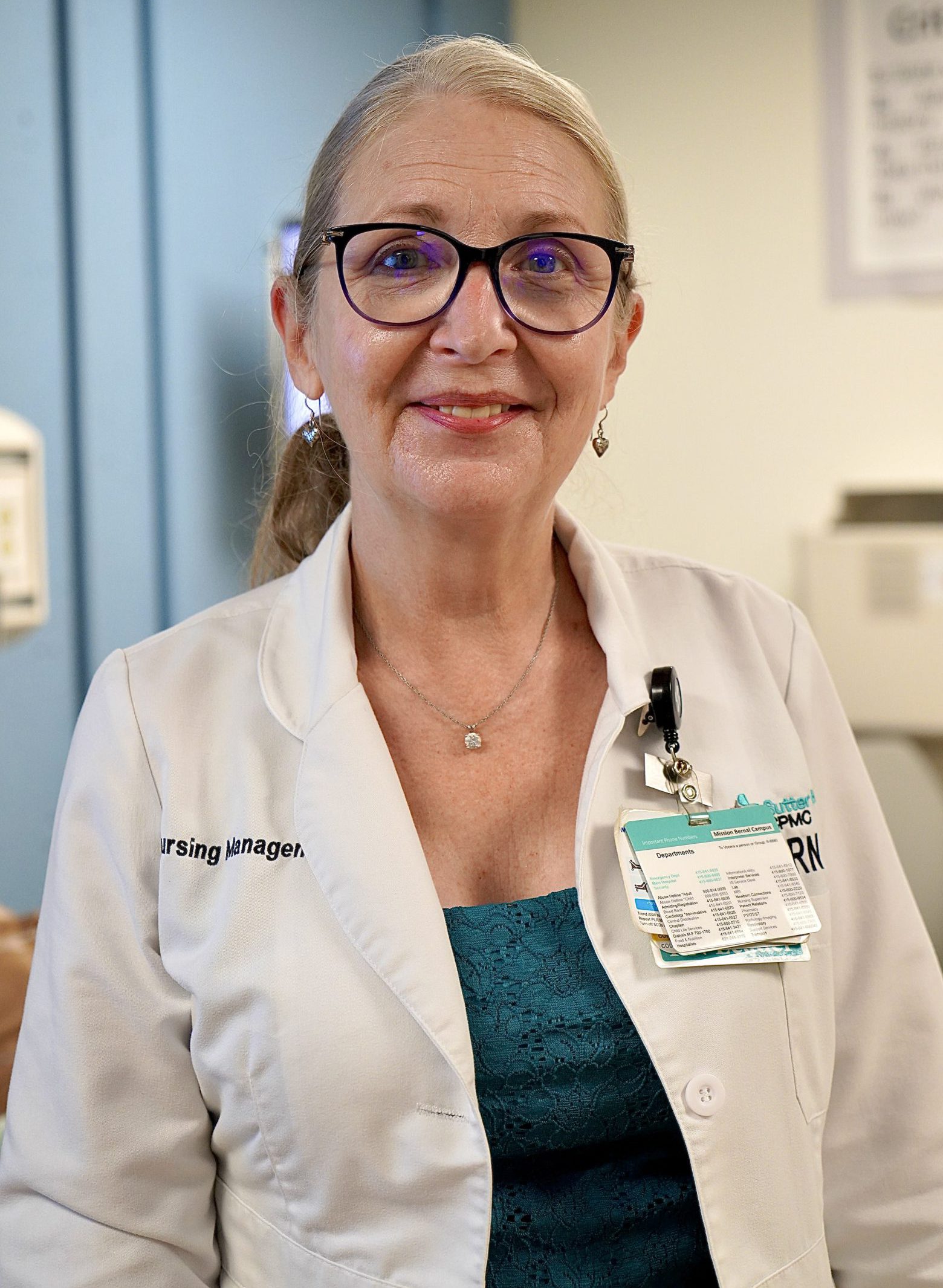
Delynn Peltz, director of nursing practice and quality at Sutter’s CPMC
Emily Martin, a clinical nurse educator who helps facilitate the camp, says the program is a safe learning environment where exercises stimulate nurses’ curiosity and their ability to think critically.
A bedside nurse is often the first on the care team to identify changes in a patient’s condition, explains Martin. “Mastery of the fundamental skills and tasks allow nurses to recognize changes and rescue patients,” she says. These abilities also help drive the clinical interventions that lead to improved patient outcomes and the delivery of consistent high-quality care.
“Competency Camp helps us feel comfortable and confident in the work we do,” says Mary Blanchard, an RN on CPMC’s medical-surgical intensive care unit. A nurse for more than 20 years, Blanchard says the day is structured in a supportive environment where asking questions is encouraged. She adds that refreshing on the basics and learning new best practices is important because “patient care is always changing and advancing.”
Applying clinical reasoning beyond the task
Twenty nurses participate in each daylong camp session at CPMC’s Mission Bernal campus. Small groups rotate through four learning areas — a simulation laboratory, equipment training, case studies and independent learning.
Building on last year’s first-ever Competency Camp, this year’s focus is on the respiratory–cardiovascular system.

CPMC nurses practice skills on a high-fidelity medical manikin in the hospital’s simulation laboratory.
Nurses this year receive practice in proning (turning a patient from their back onto their stomach) — a skill especially important for many COVID-19 patients — placing IVs and using rapid infusion devices. Groups also discuss case studies where they tap into their knowledge, experience and provide evidenced-based reasoning to identify patient conditions.
Teams also practice head-to-toe assessments using a high-fidelity medical manikin capable of breath, producing a palpable pulse, talking, coughing and more.
Delynn says every group sees, hears and reads identical information to ensure continuity, which is why the four experience rooms are scripted.
The rooms are also led by fellow CPMC nurses and not unit managers.
“Being taught by trained peers builds trust and rapport across nursing units,” says Delynn. While it may feel uncomfortable to “perform” in front of one another, she says this process allows nurses to “own” their work and understand the why of what they’re doing.
Continuing education opportunities
Sacramento-based Sutter Health offers its more than 16,000 nurses many opportunities for growth and development within the profession. Sutter Health University, based in Roseville, Calif., plays a critical piece in how the not-for-profit health system conducts such efforts.
“Nursing education is the foundation of good patient care,” says Anna Kiger, Sutter’s chief nurse officer. “The organization is committed to offering our thousands of nurses training for their licensure – and well beyond – to help them grow, learn and positively impact patients’ health and healing.”
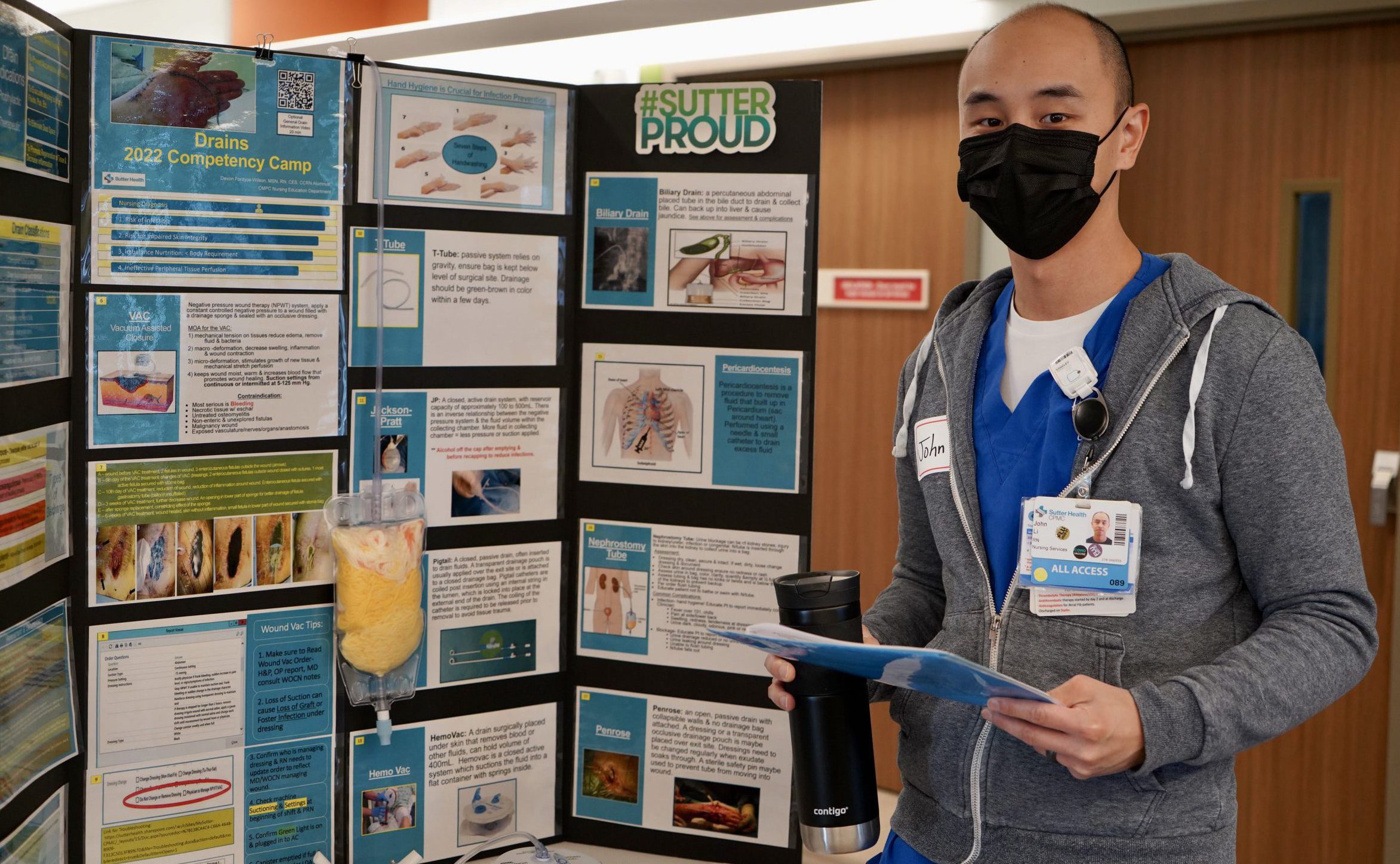
Registered nurse John Li engages in intendent learning during CPMC’s Competency Camp.
CPMC’s Competency Camp program, which goes further than typical nurse “skills days” at hospitals and health systems nationwide, is funded through donor giving.
According to Delynn, “Competency Camp is a gift to nurses in that CPMC is paying to pour into them the skills and training needed to be their very best. The only expectation in return is that our nurses give every patient the highest quality care they can possibly give.”





