By Lena Kauffman, Vitals contributor
When Martin Hyland awoke from his procedure in the neuro intensive care unit at Sutter Health’s California Pacific Medical Center’s Davies campus, he was amazed to find his body and mind functioning as if the massive stroke he’d just experienced had never happened.
Hyland had a basilar artery occlusion, one of the most disabling and deadly types of strokes. It occurs when a large blood clot shuts off oxygen to the brainstem.
Hyland was fortunate his stroke happened in the presence of friends who recognized his symptoms. He was also minutes from CPMC, where doctors are skilled at performing thrombectomies. This advanced form of less invasive brain surgery can remove deadly clots in the brain that intravenous clot-busting drugs alone may not help dissolve. If performed quickly, the technique can minimize or prevent disability and save lives.
“I didn’t realize the stroke was happening, but my friend who was talking to me asked if I was feeling OK. I said yes, but they saw I was not,” Hyland says.
Hyland’s friends called an ambulance, which arrived in six minutes. It was then a six-block ride to CPMC where Hyland was rushed to diagnostic imaging for a head CT. The scan showed the blood clot lodged in the artery to his brain stem.
“It was the most extraordinary thing,” Hyland says about going into surgery thinking he might be left severely disabled or die. “I woke up with no signs anything happened other than a bandage near my groin.”
1,000th CPMC Thrombectomy Shows Importance of Stroke Awareness

Dr. Fabio Settecase
Hyland was lucky in many ways, including that his extraordinary case was the 1,000th thrombectomy performed by the CPMC neurointerventional team. Often cases like his do not turn out as well because there are delays in receiving treatment, explains Dr. Fabio Settecase, the neurointerventional radiologist who performed Hyland’s thrombectomy.
According to Dr. Settecase, “By the time patients having a basilar artery occlusion arrive at a hospital, they may be falling into a coma and need to be intubated to keep them breathing. Hyland was still awake and able to understand what was being said to him.”
“Time is brain” is a common saying in stroke treatment, and despite the misfortune of having such a serious stroke, everything else was going in Hyland’s favor the day of the stroke.
“First, he’d not been alone when his stroke happened,” says Dr. Settecase. “He’d been at a holiday party with friends when, after a couple of sips of champagne, he didn’t feel right and had to sit down in a chair.”
At the hospital, the CPMC Davies emergency room physician quickly recognized Hyland was suffering from a stroke and alerted the Stroke Neurology Team. As soon as Hyland was diagnosed, he was given tenecteplase, a powerful intravenous drug that can often dissolve clots in the brain. At the same time, Dr. Settecase and the thrombectomy team were called in to set up the operating room in case the drug did not work.
Shortly after receiving the clot-busting medication, Hyland’s stroke symptoms resolved. He could speak normally and was able to move the left side of his body again. Minutes later, his symptoms returned and this time the right side of his body was affected. A second CT scan showed the clot was still there, and the team decided to perform a thrombectomy.
“I had no fear of death going into surgery,” Hyland says. “But I thought it was a very real possibility that I could wake up with a fate worse than death.”

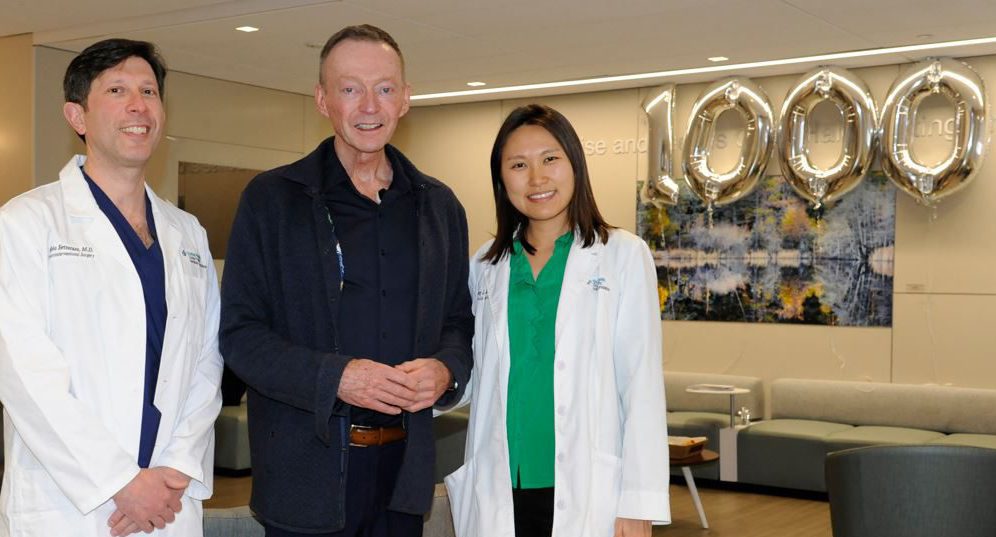
Martin Hyland stands with Sutter Health’s CPMC stroke team. Hyland’s stroke case was the team’s 1000th thrombectomy procedure.
Even doctors could only guess the outcome. Every stroke is different in the anatomy of the brain that is impacted, the amount of the clot, where the clot falls, and how long the brain cells are deprived of oxygen, Dr. Settecase explained. “There is no crystal ball on how the patients will wake up.”
How Thrombectomies Stop Strokes
Thrombectomies are performed with a catheter that snakes up from a small one-centimeter incision near the groin through the patient’s femoral artery and into their brain under X-ray guidance. Once the catheter reaches the clot, vacuum suction is applied to remove it.
Hyland was home from the hospital in two days. He felt so well that a caring friend had to gently remind him that he’d just had brain surgery and shouldn’t go back to work on Tuesday. Friends and family came in droves. “It was as though I’d fallen into a big basket of puppies of love,” Hyland says.
He acknowledges that without the quick thinking of his friends, the rapid response of the ambulance crew, and the good fortune of being taken to an advanced stroke center, he could have been severely disabled or dead. Instead, he got to celebrate his 66th birthday two weeks after leaving the hospital, enjoy the holidays with his family, and keep his planned trip to Mexico City.
Stroke Research Has Vastly Improved Outcomes

Dr. Nobl Barazangi
“Thanks to great advancements in stroke treatment over the past few decades, strokes now have better outcomes, even if there’s a delay from the start of the stroke to treatment is much greater than it was for Martin,” says Dr. Nobl Barazangi, medical director of stroke at CPMC. “However, the faster a person having a stroke can get to the right care, the better their odds for preserving brain cells and having less disability from their stroke.”
Although Hyland knew the signs of stroke well because a close friend had a stroke, he says that when it happened to him, he couldn’t recognize it and wouldn’t have been able to call 911. This is very common, Dr. Settecase says, and why it is so very important to be familiar with the signs of stroke and to promptly call for help. For example, knowing the acronym BE-FAST can save lives. It stands for:
- Balance, loss of which is one possible symptom
- Eyes, which may stop working or tracking normally
- Face, which may droop on one side or have an uneven smile
- Arm, which may be weak on one side
- Speech, which may be garbled or not make sense
- Time, a reminder to get emergency help 9-1-1 right away even if you are unsure if it is a stroke
The other important thing people should know is that the time window for when stroke medicines and procedures can help has increased greatly in the last decade, in part due to research done right here at CPMC. Dr. Joey English, director of CPMC Neurointerventional Surgery and re-searcher, started the thrombectomy program at CPMC in 2012 when new advancements in technology made it more feasible to remove large blood clots in the brain during a stroke.
Research trials at CPMC, including other hospitals across the world, showed thrombectomies improved patient outcomes even as late at 24-hours from the first symptoms of the stroke.
Dr. Joey English
“We have been on the forefront of pioneering the identification, triaging and treatment of these severe stroke patients at Sutter Health,” Dr. English says.
“Thrombectomy is becoming a more common, widespread procedure, but they are still used carefully,” Dr. Barazangi adds.
Even less invasive brain surgery is still brain surgery and has risks. That is why the team was hoping Martin’s stroke might have resolved with medication alone. In other cases, they look carefully at the size and placement of the clot, along with the brain cell damage they can see on scans, to determine what will be the best course of action for the patient.
“It is not just having the blood clot, it is making sure they will benefit from the procedure and not have harm from the procedure,” Dr. Barazangi says.
Hyland, as the 1,000th thrombectomy patient at CPMC, illustrates how this procedure done quickly by an experienced team under the right conditions, can be life changing for a patient. Only a decade ago, Hyland ’s outcome from his stroke would have been very different indeed.
“I owe it to my friends who acted so quickly and I’m very fortunate they brought me to CPMC,” Hyland says.